The use of interventional radiology procedures to treat patients for arteriovenous malformation (AVM) is less effective for those who are also heavy smokers, according to a study published July 30 in Radiology. Heavy smokers had rates of AVM relapse that were three times as high as nonsmokers.
The study focused on individuals with hereditary hemorrhagic telangiectasia (HHT), an inherited disorder in which some blood vessels don't form properly. People with HHT often form blood vessels without capillaries in the space between arteries and veins; this can make it more likely that blood vessels will form AVMs. As a result, people with HHT are much more likely to experience pulmonary AVMs, according to a research group led by Dr. Mustafa Haddad of the Mayo Clinic in Rochester, MN (Radiology, July 30, 2019).
Interventional radiology treatment with an endovascular embolization technique has emerged as an effective therapy for pulmonary AVMs, using a variety of coils and plug-like devices that are placed at the site of a malformation under imaging guidance. But such procedures can be undermined by persistence, the term for when a connection is re-established between a vein and artery despite treatment to block the interface.
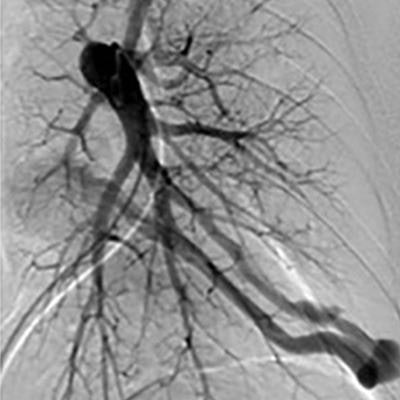
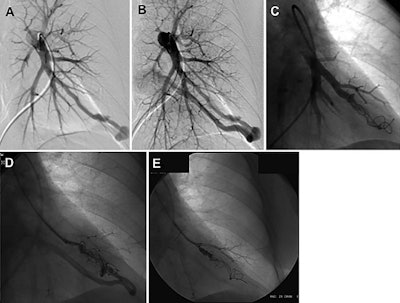 Images in a 52-year-old woman with HHT demonstrating on left pulmonary artery angiogram an AVM at the left base (A, B). Selective angiogram after embolization of the AVM by using coils (C). Angiogram shows embolization for persistence treated with repeat embolization performed two years after initial embolization (D, E). Images courtesy of RSNA.
Images in a 52-year-old woman with HHT demonstrating on left pulmonary artery angiogram an AVM at the left base (A, B). Selective angiogram after embolization of the AVM by using coils (C). Angiogram shows embolization for persistence treated with repeat embolization performed two years after initial embolization (D, E). Images courtesy of RSNA.Smokers, in particular, have a higher likelihood of persistence following endovascular treatment for AVMs, the authors noted. Smoking contributes to inflammation by disrupting vascular angiogenesis, and remodeling and promoting the chance of thrombosis. Chemicals in tobacco smoke can also contribute to oxidative stress that predisposes patients to vessel wall injury and accelerated atherosclerosis.
The authors, therefore, decided to investigate whether the effectiveness of endovascular embolization varied in individuals with HHT based on their smoking history. The team examined patients who were treated for pulmonary AVMs from 2000 to 2017, ending up with 103 individuals who met all the study's inclusion criteria. The median age of the study cohort was 52 years, and 37.9% were men; median follow-up was 6.2 years. A total of 373 pulmonary AVMs were treated in the study population, as many individuals had more than one malformation.
The researchers found that primary persistence (persistence that occurs after the first embolization procedure) occurred in 61 cases of the pulmonary AVMs, with a five-year cumulative incidence of 17.3% across the entire study group. But persistence rates varied sharply based on smoking status, the researchers found, with heavy smokers (greater than 20 pack years) having a persistence rate that was three times that of nonsmokers and a hazard ratio for persistence nearly five times that of nonsmokers.
| Persistence rates for pulmonary AVMs by smoking status | ||||||
| Nonsmokers | Smokers ≤ 20 pack years | Smokers > 20 pack years | ||||
| Persistence rate | Persistence hazard ratio | Persistence rate | Persistence hazard ratio | Persistence rate | Persistence hazard ratio | |
| Rate of primary persistence at 5-year follow-up | 12.2% | NA | 21.9% | 1.2* | 37.8% | 4.8 |
The persistence rate continued to be higher for smokers compared with nonsmokers when persistence after repeat interventional procedures were performed. Therefore, smokers should consider quitting the habit before undergoing interventional treatment for their condition.
"Smoking creates an inflammatory response," said Dr. Sanjay Misra, an interventional radiologist at the Mayo Clinic and senior author of the study. "More inflammation creates a greater likelihood of failure for smokers compared to those who never smoked. Smoking cessation is very important if these patients want to help themselves and avoid further procedures."