It was less than a decade ago that interventional radiologists reported their first experience with a new procedure for treating noncancerous but symptomatic uterine fibroids, or leiomyomas.
French practitioners had been routinely embolizing the uterine arteries of patients scheduled for myomectomy -- seeking to reduce hemorrhage during the subsequent surgery -- when they noticed that embolization itself tended to shrink the problematic fibroids. Surgeries were canceled and a less-invasive treatment was born.
Worldwide as many as 35,000 uterine fibroid embolizations (UFE), also known as uterine artery embolizations (UAE), have been performed since then, and the pace quickens every year. Yet UFE procedures are still dwarfed by long-standing surgical approaches in the U.S., where every year some 200,000 women undergo myomectomy or hysterectomy for fibroids.
 |
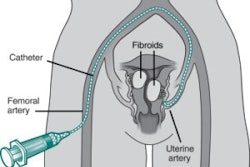
| A basic diagram of a UFE procedure. A nick is made in the skin and a catheter is inserted into the femoral artery. The catheter, which is guided through the artery with real-time imaging, releases tris-acryl gelatin microspheres into the blood vessel feeding the fibroid. Image courtesy of SIR. |
Interventional radiologists believe many of these patients would be good candidates for UFE, but the situation is déjà vu all over again for radiology. That is, the physicians who "control" most of these patients generally don’t refer them out.
The American College of Obstetricians and Gynecologists describes UFE as investigational in its most recent practice bulletin on the subject, even though an embolic agent specified for UFE was approved by the FDA in November. There are also indications that many gynecologists aren’t even mentioning UFE to patients as a treatment option -- an omission that some observers view as a violation of informed consent (Clinical Management Guidelines for Obstetrician-Gynecologists, May 2000, No. 16).
On the other hand, UFE is a relatively new procedure. So until recently, clinical studies of its performance have been inherently small and sometimes unflattering.
"I think there is valid scientific caution on the part of gynecologists," said Dr. Evan Myers, an associate professor of obstetrics and gynecology at Duke University Medical Center in Durham, NC, and a leading public health expert on fibroids.
"But there’s always a bit of a turf battle that goes on," Myers said. "This is not the first, and not the last time that a new specialty has come out with a procedure or treatment in an area that has traditionally been that of another specialty."
The resistance among gynecologists has already spawned a mini-revolution in radiology practice, inspiring more interventionalists to obtain hospital admitting privileges or develop clinics so they can treat the many UFE patients who self-refer.
"It has basically forced us into a situation of providing a full clinical service," said Dr. J. Mark Ryan, an interventional radiologist at Duke. "We now have gone back to our roots of being real clinical doctors who do ward rounds."
In a presentation at the 2003 Society of Interventional Radiology (SIR) meeting in Salt Lake City, Ryan described his department’s relationship with the ob/gyns as "acrimonious." As a result, his team has developed and implemented their own post-UFE pain management protocol without any input from gynecological colleagues (Radiology, August 2002, Vol.224:2, pp.610-613).
"(UFE) allowed us to develop an office practice with consultations and see patients outside of the hospital, which we hadn’t done before," said Dr. Neal Joseph, director of the two-year-old South Florida Fibroid Center in Hollywood. "Now, in addition to seeing several fibroid patients every office day, we’re seeing peripheral vascular patients, renal patients, oncologic patients, aortic stent graft patients -- all for consultations."
Encouraged by the success to date and the substantial upside potential of UFE, the interventional radiology community is working to win more hearts, minds, and patients. Major initiatives include research that will hopefully sway gynecologists or at least negate their objections, national information campaigns to educate physicians and the public about the procedure, and local direct-to-consumer marketing by individual practitioners and radiology groups.
Quiet epidemic
A major reason for the successful consumer marketing of UFE is that so many patients are suffering immensely from fibroid symptoms. These include pain and very heavy bleeding that can cause anemia and keep women from work and other activities. Initial treatment generally involves oral contraceptives or non-steroidal painkillers, although these are often insufficient.
Interestingly, although fibroids are by definition a problem of the childbearing years, removing the uterus is the most common surgical solution. Fewer than 40,000 myomectomies occur each year in the U.S., compared to the 150,000 or more hysterectomies performed annually for the treatment of fibroid symptoms.
In fact, U.S. hysterectomy rates have declined only a little over the last two decades, and remain three times higher than rates in Australia and western Europe, according to an analysis published last year in the American College of Obstetrics and Gynecology’s peer-reviewed journal (Obstetrics & Gynecology, February 2002, Vol. 99:2, pp. 229-234).
"The drivers for innovation tend to be either industry or physician groups," noted gynecologist and researcher Myers. "Hysterectomy cures the problem, so there hasn’t been a huge demand, at least from physicians, for alternative treatments."
At the same time, myomectomy has been far from definitive. Unlike UFE, which is designed to cut off the blood supply to all fibroids, surgeons confronted with multiple fibroids at myomectomy must choose which few to tackle. Interventional radiologists say that many of their UFE patients have previously undergone myomectomy.
"What we see very often is that the fibroids rapidly go back," says Dr. Steven Janney Smith, director of interventional radiology at LaGrange Hospital near Chicago. "It almost seems like when you take fibroids out with myomectomy, you just make more room for the little fibroids."
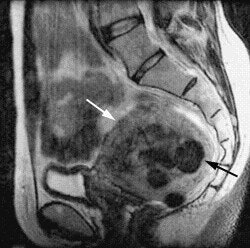
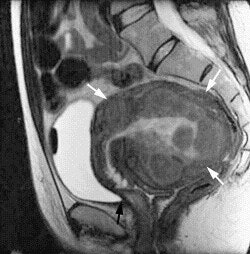 |
| This pre-embolization, sagittal T1-weighted midline MR depicts an enlarged uterus with multiple fibroids highlighted by white arrows. The black arrow points out the uterus impinging anteriorly on the bladder neck. Image courtesy of Dr. Steven Janney Smith. |
Many myomectomy patients end up having a hysterectomy. But interventional radiologists suggest that gynecologists may have underestimated the number of patients who want to preserve their fertility, or who have a cultural or personal aversion to hysterectomy.
"What I’ve heard many, many times is, ‘I just don’t want to lose my uterus. To me it would feel like a castration,’" Ryan said.
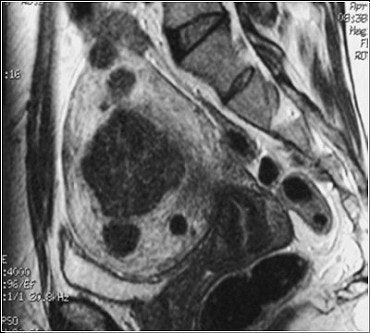
 |
| The same patient six months after the UFE procedure. This sagittal, T1-weighted midline MR image shows a 50% decrease in the size of the uterus (white arrow). The fibroids have low signal (black arrow), consistent with devascularization. The patient reported complete relief of symptoms. Image courtesy of Dr. Steven Janney Smith. |
Patients are also self-referring for the other benefits of UFE, interventionalists said. As with most interventional radiology procedures, UFE is less invasive than the surgical alternatives. A catheter is inserted into the femoral artery and is threaded to the uterine arteries, where embolizing particles of plastic or gelatin are released. Hospitalization is usually one night.
After UFE most women can resume normal activity within a week, a shorter time than some myomectomy approaches and definitely shorter than the standard six-week recovery after hysterectomy. The shorter recovery time is appealing for working women and those with families.
Physician shift
Given the pokey evolution of gynecology’s fibroid treatments, it’s probably not surprising that gynecologists have been slow to even acknowledge the availability of UFE. But change is occurring.
After interventional radiologists at Yale University in New Haven, CT, began offering UFE in 1998, they started tracking gynecologists’ opinion of the procedure by asking patients about the advice they received. Among women who underwent UFE at Yale between 1998 and mid-2000, only 10% had learned about the procedure from their gynecologists.
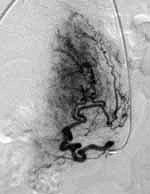 |
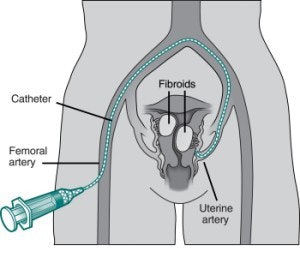
| Pre-UFE angiogram with catheter insertion. Contrast highlights fibroids. Image courtesy of Dr. Neal Joseph, Radiology Associates of Hollywood, FL. |
By mid-2000 to 2002, some 43% of the patients treated had heard about UFE from their gynecologists. But that increase doesn’t placate the researcher who presented the latest findings to the Society of Interventional Radiology.
"A majority of gynecologists still are not offering uterine fibroid embolization as an option," said Elizabeth K. Arleo, a third-year Yale medical student. "It’s disconcerting, because informed consent dictates that all possible treatment options should be mentioned."
 |
| The post-UFE image shows arteries occluded for a reduction in blood flow to the fibroids. Image courtesy of Dr. Neal Joseph, Radiology Associates of Hollywood, FL. |
Financial self-interest is the driving issue, contends Yale interventionalist Dr. Michael Tal. "The obstetrics is not as lucrative and there’s a lot of malpractice (insurance costs), so hysterectomy is one of the main sources of income for gynecologists."
Whatever self-interest they may have, gynecologists are changing their stated position on UFE. Only 33% of the gynecologists described in the latest Yale survey were opposed to UFE when it was raised as a treatment option, compared to 76% two years earlier.
Interestingly, gynecologists may take a financial hit if they oppose UFE: The research also found that patients who underwent the procedure despite their gynecologist’s opposition were very unlikely to see that gynecologist again.
Patients first
The evolving opinions of gynecologists probably reflect their increasing familiarity with UFE, both from national and local sources, Tal said. There have been more journal articles and news reports, and Tal has spoken directly to gynecology groups about UFE.
"Initially, the patients that you will get based on those presentations are the patients that nobody wants to operate on," Tal said, citing patients with HIV, hepatitis, obesity, and other comorbidities. Still, "every patient is a way to capitalize on building a relationship with that specific gynecologist."
So with every case, Tal sends the gynecologist copies of all pre- and post-procedure clinical notes. "The key thing in building a UFE practice, in my opinion, is to take responsibility for the patient before, during, and after the procedure, and, while doing this, maintain a positive and open communication with the gynecologist," he said.
Even if interventional radiologists have initially taken on new clinical responsibilities because gynecologists refused to work with them, continuing with this approach seems logical and appropriate.
"A model where the gynecologist refers the patient to the IR -- who then does the procedure and the gynecologist then handles all the problems afterward -- isn’t going to be very attractive," said gynecologist Myers.
 |
| Getting back to basics: Dr. Michael Tal steps out of the interventional suite to talk with a patient about her UFE options. Often a woman’s ob/gyn won’t even entertain the subject, so it may be up to the interventional radiologist to take over. Image courtesy of Dr. Michael Tal. |
Interventionalist Smith agreed: "Why should I make them admit the patient and do all this if I’m getting paid to do the procedure? It’s not fair to them."
Total responsibility for the patient also empowers interventionalists to provide the kind of service that generates good buzz.
"Making sure there are no stones left unturned, making sure that you are treating the patient for post-procedural pain adequately -- basically making a good experience for patients," said Ryan. "I think that has been extremely important."
Consumer marketing
Attention to detail does more than generate word-of-mouth business, Ryan says. Women also share their experiences in Internet health chat rooms that spread the word much farther and wider.
In fact, the Internet appears to be critical in enabling UFE to avoid the fate of other new procedures that challenged entrenched approaches. "Women find out information on the Internet and they know what they want," said Tal. "So the gynecologists have to, and do, adapt to that."
Interventionalists also credit the Web sites developed for their practice groups with bringing in numerous self-referred patients. "Without it I don’t know how we would have ever gotten started, since right out of the box we were kind of viewed as a threat to the livelihood of gynecologists," said Smith.
As a new marketing tool for doctors, the Internet also presents some headaches. For instance, Smith was somewhat chagrined when the Web site developer he hired selected DrFibroid.com as the Internet address. "It sounds like I’m a used-car salesman," he complained. But Smith kept the name because at that point, he didn’t know that he could choose another.
 |
| The SIR advertising campaign, marketing UFE directly to patients, generated a significant increase in the number of procedures performed. Image courtesy of SIR. |
Other approaches that interventionalists have used to reach patients include speaking to women’s groups and inviting local television or newspaper reporters to see a procedure and interview previous patients.
Then there is the marketing used by Joseph for the opening of the South Florida Fibroid Center in 2000. With help from a consultant who had promoted the University of Miami’s medical facilities, the fibroid center ran advertisements in major daily newspapers, on cable television, and on two radio stations whose listeners matched the demographics of fibroid patients.
The two-month ad campaign worked so well -- especially the radio spots, which generated 90% of the self-referrals, Joseph said -- that the center did it again a year later.
"We already had a good baseline, but it gave us another boost of patients," said Joseph, who also had anecdotal evidence that his 30-second descriptions of fibroid symptoms and treatment were being heard during drive time. "I’d come to work and everybody was saying, "Oh, I heard you on the radio."
The South Florida Fibroid Center is now handling 20 to 25 embolizations a month. Joseph says that results have also influenced his colleagues at Radiology Associates of Hollywood. "It’s just got us into the habit of marketing ourselves and our practice both to physicians and to the public," he said.
National news
In addition to the marketing by individual UFE practitioners, SIR recently completed a yearlong public information campaign that included ads in Ebony magazine, the Journal of Family Practice and Annals of Internal Medicine, and dissemination of video and print press releases and public service announcements.
The campaign generated significant increases in traffic to SIR’s call center and Web site: Phone inquiries went up from 45 to 200 per month, and hits on the Web site’s UFE "physician finder" went from 25-33 per day to as high as 81 in one day.
Demand for SIR’s information has slowed with the conclusion of its campaign, although the society continues to provide patient and physician "Grand Rounds" information both on its Web site and as handouts for use by its 3,000 members.
The education effort has also been picked up by BioSphere Medical, a Rockland, MA, company that received FDA approval of its acrylic co-polymer embolizing beads in November. BioSphere is now advertising a toll-free hotline (1-877-ASK-4UFE) and Web site ( www.ASK4UFE) through the New York Times and the Wall Street Journal.
But mass marketing doesn’t always fit comfortably with medicine.
"The problem with any kind of direct-to-patient marketing (by physicians) is there’s no real oversight of the validity of claims," Myers said. "Historically, new innovations tend to get marketed very aggressively, and gynecologists have been guilty of that as well with various laparoscopic procedures."
Judging UFE
Interventional radiologists agree that their procedure should be validated through traditional scientific scrutiny, although many argue that the medical literature already makes an excellent case for UFE’s safety and efficacy. After all, embolization of the uterine arteries has been performed for more than 25 years to stem postpartum hemorrhage, with studies showing successful treatment and subsequent pregnancies among the patients.
SIR recommends providing referring physicians with studies published in their specialty journals, such as the series of reports in Fertility and Sterility on the Ontario Uterine Fibroid Embolization Trial, a prospective multicenter study of 555 UFE patients.
Another popular citation is an article in Obstetrics and Gynecology by Dr. James Spies and colleagues at Georgetown University in Washington, DC. It reported on 400 consecutive patients who underwent embolization, with serious complications for only 1.25% and a 5% overall periprocedural morbidity rate (July 2001, Vol. 98:1, pp. 29-34).
Other articles have reflected less favorably on UFE, including a UCLA study that found that women were more likely to need further invasive treatment after UFE than after myomectomy (Obstetrics and Gynecology, November 2002, Vol. 100:5, part 1, pp. 864-868).
Thus, many UFE providers are participating in further research to confirm their perception of the procedure. Foremost among these is the FIBROID registry spearheaded by SIR’s Cardiovascular and Interventional Radiology Research and Education Foundation (CIRREF). This registry now includes data on more than 3,000 patients treated at dozens of sites around the world.
In a talk at the 2003 SIR conference, Dr. Robert Worthington-Kirsch from the CIRREF FIBROID Registry Steering Committee shared the latest data on patient demographics and procedure techniques. Boston Scientific of Natick, MA, and Biosphere provided research funds for the multicenter registry. Both companies manufacture embolic microspheres used in UFE.
| This pre-UFE, sagittal FSE MR image depicts a large submucosal fibroid and several small intramural fibroids. Image courtesy of Dr. J. Mark Ryan. |
"As of August 31, 2002, we have 2,605 cases logged," Worthington-Kirsch said. "Of those 2,605 patients, 2,471 have given consent for long-term follow-up, and 2,300 cases were available for analysis. Registry enrollment closed after the first of January with somewhat over 13,000 patients enrolled. Data has been provided from 58 sites, 52 in the U.S., four in Canada, one in the U.K., and one in Hong Kong."
The mean age of the women undergoing UFE was 43.4 with Caucasians and African-Americans making up the bulk of the patient population. Comorbidities included obesity, smoking hypertension, and diabetes. In terms of reproductive history, just under half had never had a child, he said.
"Just over half the patients were evaluated by MRI, and half the patients were evaluated by either transabdominal or transvaginal ultrasound. The mean uterine volume was just under 1,300 cc with a reasonable spread. Half the patients had one or two fibroids; about a quarter of the patients had five or more fibroids," Worthington-Kirsch said. The majority of patients (85%) complained of menorrhagia. Other symptoms included bulk or pressure and pain.
 |
| This sagittal FSE MR image, one-year post-UFE, shows a marked reduction in uterine volume and almost complete shrinkage of the submucosal fibroid, as well as a decrease in the size of intramural fibroids. Image courtesy of Dr. J. Mark Ryan. |
In terms of technique, the primary embolic agent used was calibrated microspheres in just under 75% of the patients, he reported. In just over half the patients, microcatheters were used with an average of about 1.2 catheters per case.
"The mean procedure time was about 55 minutes; the mean fluoroscopy time was 16.3 minutes, and this agrees with other procedures of similar difficulty and complexity," Worthington-Kirsch said. "An average of 64 angiographic images were obtained. The overall technical success was 98%, with both uterine arteries embolized. Just about everybody received (intravenous) conscious sedation during the procedure and then most received PCA (patient-controlled analgesia) narcotics afterward for pain management." The average hospital stay was 1.4 days.
The principal investigator for the FIBROID registry is Duke gynecologist and researcher Myers. He says the database will enable some good conclusions about the safety of UFE, as a start. But it won’t necessarily enable comparisons with other fibroid treatments.
Myers summarized the problem as lead author of a 2001 report by the U.S. Agency for Healthcare Research and Quality on management of uterine fibroids: "In general, there was a remarkable lack of high-quality evidence supporting the effectiveness of most interventions for symptomatic fibroids."
Still, winning over gynecologists will probably require radiologists to demonstrate their initiative as researchers as well as clinicians. "I think if there was good data that this was equivalent to myomectomy, it would be harder for there to be resistance," Myers said.
Duke’s Ryan is among the interventional radiologists looking to do a head-to-head trial, assuming that gynecologists will participate after he publicly criticized their attitude toward UFE.
"You know Osama bin Laden? Well, I came next on the list, pretty much," said Ryan of the reaction he received. "But things have evolved, and there’s been generation of mutual respect and greater appreciation of what we as interventional radiologists do."
By Tracie L. ThompsonAuntMinnie.com contributing writer
June 13, 2003
Additional reporting by Shalmali Pal.
Related Reading
Boston Scientific inks deal for device-tracking technology, May 19, 2003
Uterine fibroid embolization does not impair fertility, April 1, 2003
Women respond well to UAE in the long term, SIR study shows, March 29, 2003
GE rolls out Innova 4100, March 28, 2003
MR helpful in managing patients with uterine fibroids, January 23, 2003
Cheaper UAE edges out hysterectomy for uterine fibroid treatment, January 17, 2003
BioSphere gets FDA clearance for UFE microspheres, November 27, 2002
Copyright © 2003 AuntMinnie.com