Whole-body diffusion-weighted MRI (DWI-MRI) appears to help clinicians effectively assess tumor response to chemotherapy in children, according to a study published May 5 in Radiology.
The findings offer a modality that doesn't use ionizing radiation as an alternative to current approaches such as FDG-PET/CT for evaluating pediatric cancer treatment response, wrote a team led by Dr. Heike Daldrup-Link, PhD, of Stanford University.
"[Our study raises] the possibility that [DWI-MRI] might one day be used in place of CT scanning, either together with FDG-PET or alone, without the need to inject radioactive glucose," the group noted. "This new approach could reduce radiation exposure by 80% for combined [FDG-PET/DWI-MRI] and fully eliminate radiation exposure for tumors that can be evaluated with [DWI-MRI] only."
Cancer therapies for children have improved, leading to an increased number of survivors. But tracking the effectiveness of cancer treatment and even follow-up using PET/CT exposes children to more radiation, which puts them at risk of secondary cancers. Although previous studies have shown that DWI-MRI can detect cancer, it's been unclear whether it can accurately monitor treatment response, the group noted.
To address this question, Daldrup-Link and colleagues compared DWI-MRI with FDG-PET/CT in 56 patients with lymphoma or sarcoma (mean age, 15; range, six to 22) who simultaneously underwent 112 whole-body DWI-MRI exams and FDG-PET/MRI scans -- one before treatment began and then another after the first few weeks of chemotherapy.
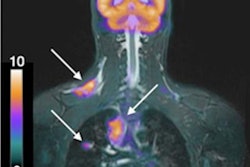
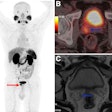
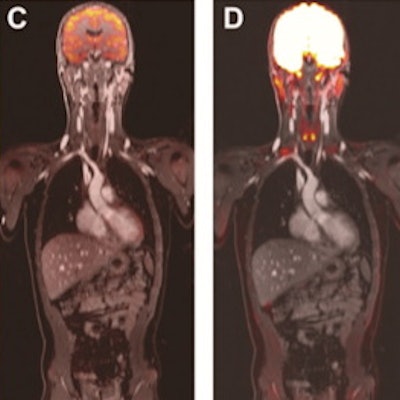
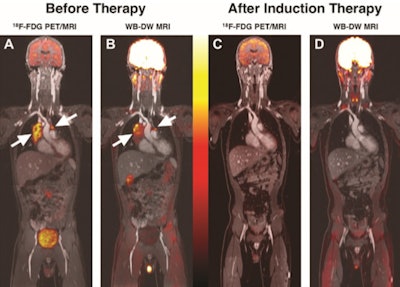 Concordant information with FDG-PET/MRI and whole-body DWI-MRI for monitoring treatment of diffuse large B-cell lymphoma. A, Coronal color-encoded fused FDG-PET/MRI scan and, B, color-encoded fused whole-body DWI-MRI scan obtained before chemotherapy in a 13-year-old boy with diffuse large B-cell lymphoma show FDG- and DWI-positive mediastinal lymph nodes (arrows). C, Coronal color-encoded fused FDG-PET/MRI scan and, D, color-encoded fused whole-body DWI-MRI image obtained after induction therapy show complete treatment response. Images courtesy of the RSNA.
Concordant information with FDG-PET/MRI and whole-body DWI-MRI for monitoring treatment of diffuse large B-cell lymphoma. A, Coronal color-encoded fused FDG-PET/MRI scan and, B, color-encoded fused whole-body DWI-MRI scan obtained before chemotherapy in a 13-year-old boy with diffuse large B-cell lymphoma show FDG- and DWI-positive mediastinal lymph nodes (arrows). C, Coronal color-encoded fused FDG-PET/MRI scan and, D, color-encoded fused whole-body DWI-MRI image obtained after induction therapy show complete treatment response. Images courtesy of the RSNA.The team measured tumor apparent diffusion coefficients (ADCs) and maximum standardized uptake value (SUV) of up to six lesions using the area under the receiver operating curve measure, as well as the agreement between the two techniques using Krippendorff's alpha coefficient (with agreement higher the closer the measure is to 1).
The researchers found that both methods produced similar results in assessing treatment effectiveness, with an agreement value of 0.88 (agreement was higher in patients with sarcoma, at 0.94, than in patients with lymphoma, at 0.74). FDG-PET identified treatment response sooner than DWI-MRI in eight of 56 patients (p = 0.002).
| Performance comparison, FDG-PET/MRI vs. DWI-MRI for tracking cancer treatment response | ||
| Performance measure | FDG-PET/MRI | DWI-MRI |
| Sensitivity | 100% | 96% |
| Specificity | 100% | 100% |
They also found that chemotherapy response prediction according to maximum SUV and minimum ADC were similar between the two techniques when measured by area under the receiver operating characteristic curve, with a p value of 0.37.
The study findings are promising, but more research is needed, according to Dr. George Giacoia of the U.S. National Institutes of Health's (NIH) Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), which funded the study.
"Advances in pediatric cancer treatment have led to more survivors, but radiation exposure from current imaging techniques raises the risk of new cancers later in life," he said in a statement released by the NIH. "These initial results on [DWI-MRI] are promising, but they need to be confirmed by additional studies."