Post-therapy SPECT/CT scans after cycle 2 of lutetium-177 prostate-specific membrane antigen-617 (Lu-177 PSMA-617) predict overall survival in patients with advanced prostate cancer, according to a study published July 3 in the Journal of Nuclear Medicine.
The finding is from a retrospective analysis of scans from participants in three clinical trials and suggests that post-therapy SPECT/CT may improve treatment strategies for patients with poor prognoses, noted lead author Raghava Kashyap, MD, of the University of Melbourne in Australia, and colleagues.
“Identifying this subgroup of patients with [metastatic castration-resistant prostate cancer] with poor outcomes may facilitate strategies for treatment intensification to improve outcomes or transition to the next treatment or to best supportive care,” the group wrote.
The role of post-therapy imaging is continually evolving for patients receiving therapy with Lu-177 PSMA-617 (Pluvicto, Novartis), the authors explained. Quantitative changes on posttherapy SPECT/CT scans have been demonstrated as prognostic for progression-free survival, but not overall survival, they noted.
In this study, the group assessed whether quantitative and visual changes in post-therapy SPECT/CT images can serve as prognostic biomarkers for overall survival among patients in three clinical trials conducted in Australia. Specifically, they looked at the prognostic value of two factors: changes in quantitative parameters and the appearance of new PSMA-avid metastases. They also assessed the impact of imaging on clinical management.
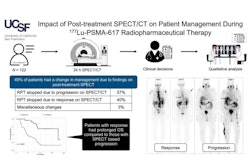
 A visual abstract of the studyJournal of Nuclear Medicine
A visual abstract of the studyJournal of Nuclear Medicine
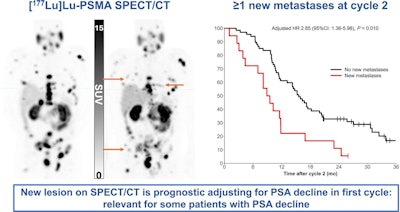
According to the results, a reduction in total lesion activity and metabolic tumor volume between cycles 1 and 2 was prognostic for overall survival on a univariate analysis, but not on a multivariate analysis when adjusting for age, Gleason score, and reduction in prostate-specific antigen (PSA). Changes in maximum standard uptake values (SUVmax) and mean SUV were not prognostic for overall survival.
However, the appearance of new lesions on cycle 2 post-therapy SPECT/CT images was prognostic for overall survival on both univariate (hazard ratio [HR], 2.38; p = 0.002) and multivariate (HR, 2.85; p = 0.01) analyses. The median overall survival for patients with new lesions was 9.2 months compared with 15.6 months for those without new lesions. Notably, 8% of patients (7/85) who had reductions in PSA levels after cycle two had new lesions detected on post-therapy SPECT/CT, the researchers reported.
In addition, post-therapy SPECT/CT was observed to have a high impact on clinical management in 20 (24%) of 85 patients. Among these, therapy was paused because of exceptional response in nine patients (11%) and was discontinued because of unequivocal progression in five patients (6%).
“The strongest prognostic parameter was the detection of new metastases after cycle 2, surpassing the value of quantitative biomarkers and being superior to clinical parameters,” the group wrote.
Ultimately, the study shows that post-therapy SPECT/CT imaging adds value in managing these patients beyond PSA or quantitative measures, as some patients develop new metastases despite decreasing PSA values, the researchers wrote. Moreover, visual analysis is rapid and does not require specialized software for image processing, they added.
“The presence of new metastases on post-therapy SPECT/CT after cycle 2 is an independent prognostic biomarker for OS in patients with mCRPC and could guide future prospective research to improve treatment strategies for patients with poor prognoses,” the researchers concluded.
The full study is available here.