From its early days 10 years ago to the present, PET/MRI has developed from a modality simply comparable to PET/CT to one that is changing clinical practice and becoming a potentially "killer application" in prostate cancer.
In a presentation at ECR 2021, researchers provided a review of recent developments in PET/MRI and considered (with apologies to "Game of Thrones" fans) whether PET/MRI is "the prince that was promised."
Today, there are about 110 hybrid PET/MRI scanners installed worldwide, with 23% in North America and 54% in Europe. A majority of installed sites split use of the scanners between applications in oncology and clinical research.
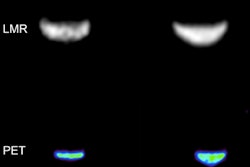
Early, small studies with the hybrid modality focused on whole-body staging and showed promising evidence that F-18 FDG PET/MRI and PET/CT provided comparable diagnostic information. But it wasn't until a larger study of more than 1,000 subjects was published in the Journal of Nuclear Medicine in 2020 that researchers began to see its potential.
 Dr. Lale Umutlu.
Dr. Lale Umutlu."In the beginning, a majority of studies focused on the comparison of PET/CT versus PET/MRI because we didn't really know how to handle PET/MRI. We didn't know how good the diagnostic accuracy would be," said Dr. Lale Umutlu, head of clinical PET/MRI at University Hospital Essen in Germany.
The JNM study showed not only that PET/MRI and PET/CT are comparable but also that PET/MRI is superior in areas they did not expect, mainly in gastrointestinal cancer, neuroendocrine tumors, gynecologic and breast cancer, and prostate cancer. PET/MRI identified 155 more cancer cases than PET/CT did.
"We did not expect PET/MR imaging to be better than CT in malignant melanoma or malignant bone disease," Umutlu said.
PET/MRI is having a significant effect on the clinical management of colorectal cancer, according to Dr. Onofrio Catalano, PhD, medical director of PET/MR at Harvard Medical School's Martinos Center. He discussed several PET/MRI case studies during the ECR session.
 Dr. Onofrio Catalano, PhD.
Dr. Onofrio Catalano, PhD."There's no other imaging modality to my eyes which can provide such a fantastic combination of information," he said.
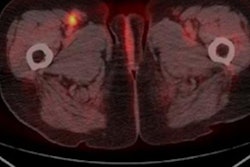
When colorectal cancer has been treated and the patient's best chance for survival is complete surgical resection, radiologists are using PET/MRI to provide a detailed assessment of the infrastructure of the disease for their surgical colleagues. Onofrio said this includes tracing roots and results in a virtual road map for the surgeons.
"PET/MRI offers higher performance compared to CT and MRI/CT in looking for recurrence in the pelvis, and can change management in even up to 35% of cases," he said.
In a study published in 2019 in the European Journal of Nuclear Medicine and Molecular Imaging, Onofrio and colleagues provided evidence that PET/MR changed clinical management compared to standard-of-care imaging in 15 out of 42 cases, distributed as follows:
- Upstaging the patient's condition, prompting surgery (11.9%)
- Upstaging the patient's condition, aborting surgery in favor of chemotherapy or palliation (4.8%)
- Upstaging the patient's condition, aborting surgery in favor of chemoradiotherapy combined with immunotherapy (4.8%)
- Downstaging, making patients resectable (11.9%)
- Downstaging, avoiding unnecessary surgery (2.3%)
Because PET/MRI is such an effective tool for assessing the local extent of disease, it is having a similar effect on clinical management of disease in the bone, liver, peritoneum, and lymph nodes, Onofrio concluded.
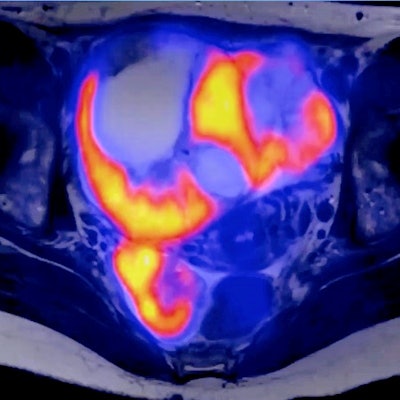
PET/MRI is on its way to being considered a "killer application" in prostate cancer, the second leading cause of cancer mortality in men, according to Dr. Marcus Makowski, director of the Institute for Diagnostic and Interventional Radiology at University Hospital Rechts der Isar in Munich.
 Dr. Marcus Makowski.
Dr. Marcus Makowski."PET/MRI is ideally suited for prostate cancer because it combines excellent anatomic and functional information of MRI and the higher specificity of PET," he said.
PET/MR improves accuracy in detecting bone metastasis and characterization in the early stages of the disease, and it is evolving in its usefulness in identifying prostate cancer lung lesions. The synergistic strength of PET/MRI in prostate cancer has high potential in imaging, especially for challenging locations.
Yet, PET/MRI has at least one limitation.
"Cost and availability are significant issues," Makowski concluded.
So, is PET/MRI the promised prince? These researchers believe so. Will it be crowned?
Umutlu predicted that phenotyping different kinds of cancer with PET/MRI will continue to advance, building on early evidence of success in breast cancer. This will allow doctors to project therapy responses and stratify patients accordingly.
Ultimately, radiologists will be able to include these virtual biopsies, as they are being called, in reports to better guide clinicians, new oncologists, and surgeons, she said.
Instead of performing invasive tissue sampling for the biopsy to assess the mutational status of tumors, maybe we will only need imaging in the future, she suggested.
"We find ourselves right now in a period of change in diagnostic algorithms," Umutlu concluded. "I think we need to be open to include computational analysis and complementary information. We have everything we need to provide the best diagnostics for our patients."