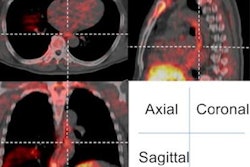
Performing PET/CT scans while patients are undergoing radiotherapy prior to surgery for esophageal cancer can help predict whether they will respond to treatment, according to a study published April 18 in Radiotherapy and Oncology.
South Korean researchers analyzed data from PET/CT scans in patients with esophageal cancer who underwent imaging about midway through radiotherapy treatment prior to surgery. They found that specific PET/CT parameters predicted how long patients survived without their cancer reappearing.
"Tumor metabolism changes during [radiotherapy] can be a useful predictive tool for treatment response and recurrence in patients with esophageal cancer," wrote Dr. Chang Geol Lee, PhD, of Yonsei University College of Medicine in Seoul.
Esophageal cancer has an extremely poor prognosis. Less than 50% of patients have inoperable status at first diagnosis, and even after surgical resection, survival rates are less than 35%. Studies have shown patients have better chances of survival when treated with a course of radiotherapy followed by surgery, rather than surgery alone.
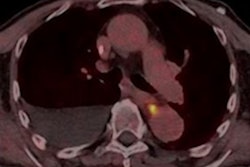
Metabolic parameters evaluated by F-18 FDG-PET/CT are known prognostic markers in various cancers. In the current study, the South Korean researchers hypothesized that measuring these parameters in patients with esophageal cancer midway through radiotherapy could predict their overall treatment response.
The researchers included 83 patients in the study who were treated with radiotherapy with or without chemotherapy and who underwent mid-therapy F-18 FDG PET/CT scans (Biograph TruePoint 40, Siemens Healthineers) between 2015 and 2020.
At their hospital in Seoul, the researchers administer definitive radiotherapy in esophageal cancer patients for six weeks and preoperative radiotherapy for four weeks. Patients in this study underwent midtherapy PET/CT scans approximately one-third of the way through radiotherapy treatment.
The median follow-up period was 10.5 months. Results indicated midradiotherapy PET parameters were significantly associated with locoregional recurrence-free rates and distant metastasis-free rates.
Among the PET parameters, the strongest statistically significant finding was the correlation between higher midradiotherapy SUVmax and locoregional recurrence (p = 0.009), according to the findings. In addition, the researcher found that a cutoff value of 11 for midradiotherapy SUVmax successfully distinguished between poor and better prognosis, the researchers stated.
"This implies the clinical significance of mid-[radiotherapy] PET in predicting not only recurrences but also treatment response, directly related to survival outcomes," they wrote.
Ultimately, early response is an indicator of tumor biology and a predictor of treatment failure, the researchers wrote. The value of PET parameters during treatment has been widely accepted in patients treated with chemotherapy for esophageal cancer, yet evaluating early response using PET/CT can be helpful in identifying patients who need either intensification or modification of treatment, they suggested.
"Clinicians may consider early response evaluation with PET during [radiotherapy] for information about prognosis," Lee and colleagues concluded.