Key information on PET/CT imaging reports on whether head and neck cancer patients are responding to radiotherapy may not be getting through to clinicians, according to a study published August 18 in JAMA Otolaryngology -- Head & Neck Surgery.
In an observational cohort study, a team of radiologists at Wake Forest University in Winston-Salem, NC, explored how clinical oncologists performed when evaluating patient response to radiotherapy (RT) based on nuclear medicine PET/CT reports. They found a significant lack of clarity among the clinicians.
"Clinician perception of patient response from the post-RT PET/CT freeform report is unreliable and does not consistently reflect the radiologist's intended meaning, which was strongly associated with survival," wrote corresponding author Dr. Ryan Hughes, an assistant professor of radiation oncology, and colleagues.
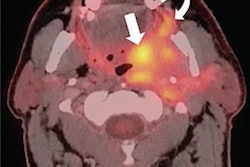
After patients with head and neck cancer undergo radiation therapy, imaging exams such as F-18 FDG PET/CT scans are used to gauge their response to the treatment. Previous research has documented discrepancies between radiologists' intended meaning as conveyed in imaging reports and clinicians' perceived meaning. These miscommunications may contribute to elevated patient anxiety, unnecessary follow-up procedures, or failure to recognize and adequately treat residual or progressive disease, according to the authors.
In this study, the researchers aimed to clarify whether that discord exists when clinicians reviewed the entire text (words and phrases only) of post-treatment PET/CT freeform reports for follow-up of head and neck cancer patients.
The researchers included 171 patients with head and neck squamous cell carcinomas (HNSCC) treated with radiation therapy at Wake Forest between January 2014 and December 2019, with a post-treatment PET/CT scan and one year or longer of follow-up. Four clinicians assigned a response category (complete, indeterminate, partial, or progressive disease) for patients based on their perceived meaning of the PET/CT report.
According to the results, the level of agreement was low among the clinicians. There was exact agreement between clinician consensus and the nuclear medicine physician's interpretation on the PET/CT reports in 81 of 124 patients determined to have a complete response, seven of 16 patients with indeterminate findings, 16 of 24 patients with a partial response, and five of 10 patients with progressive disease.
"The results of this study suggest only modest agreement between oncology clinicians' perceptions of a patient's disease status after reviewing post-treatment PET/CT freeform reports," the authors wrote.
Given the prognostic effect of post-radiation therapy PET/CT reports, accurately communicating a patient response category is essential, the authors wrote. Yet there is no universally accepted standardized method for communicating results, the authors wrote.
At Wake Forest's hospital system, however, departments recently implemented the Neck Imaging Reporting and Data Systems (NI-RADS), a standardized reporting system devised by the American College of Radiology in 2017. So far, they have demonstrated feasibility and rapid acceptance of the reporting method.
Ultimately, the group believes that implementing NI-RADS may be a cost-effective method to rapidly improve the quality of post-RT response reporting, especially since it requires minimal additional effort on the part of interpreting nuclear medicine physicians, the authors wrote.
"We now aim to perform a similar quality-improvement implementation study on the use of a systematic PET/CT reporting system for posttreatment imaging of patients treated for HNSCC," Hughes and colleagues concluded.