A novel PET imaging approach could help with earlier diagnosis and treatment for patients with progressive apraxia of speech (PAOS), suggest findings presented June 23 at the Society of Nuclear Medicine and Molecular Imaging (SNMMI) annual meeting in New Orleans, LA.
In her talk, Ryota Satoh, PhD, from the Mayo Clinic in Rochester, MN, discussed how she and colleagues found that PAOS patients have more brain inflammation than healthy individuals, especially in areas of the brain that control movement and speech.
“We believe that our findings could have a positive impact on research and development of neuroinflammatory PET techniques,” Satoh said.
PAOS is a rare neurodegenerative disorder that affects individuals' speech. Patients have a slow speech rate, distorted sound substitutions, and effortful facial movements, and they are also likely to have Parkinson-plus syndrome in the later stages.
Previous studies have shown prominent atrophy and tau uptake in the premotor cortex and subcortical structures in PAOS-affected brains. However, the researchers noted that not much is known about their neuroinflammatory profile and ties to Parkinson-plus syndrome and Tau uptake.
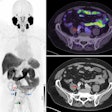
 Images depict brain regions where PAOS had greater neuroinflammation than that seen in healthy individuals.SNMMI
Images depict brain regions where PAOS had greater neuroinflammation than that seen in healthy individuals.SNMMI
Satoh and colleagues studied spatial patterns of neuroinflammation in PAOS with and without Parkinson-plus syndrome, as well as its relationship with tau uptake. The team used [C-11]ER176 TSPO PET imaging for the prospective study.
The team recruited 25 PAOS patients, 13 of whom had Parkinson-plus syndrome, and 30 individuals serving as healthy controls. All patients underwent both C-11 ER176 neuroinflammatory and F-18 flortaucipir tau PET scans.
The researchers reported the following:
PAOS patients had more neuroinflammation than the healthy control group did in the premotor cortex, superior, middle, and inferior frontal gyri, basal ganglia, and midbrain (uncorrected p < 0.001).
PAOS patients without Parkinson-plus syndrome had a more restricted uptake pattern limited to the bilateral premotor cortex and left frontal gyri (uncorrected p < 0.001).
Patients with Parkinson-plus syndrome had a broader uptake pattern extending to prefrontal, parietal, and temporal cortices (uncorrected p < 0.001).
On regional correlation analysis, there were significant positive correlations between the neuroinflammatory and tau standardized uptake value ratios (SUVRs) in 23 out of 24 evaluated PAOS patients (r = 0.56).
The researchers also found that patients with Parkinson-plus syndrome had higher correlation coefficients than PAOS patients without the syndrome (p < 0.001). And in voxel-based correlation analysis, PET SUVRs were positively correlated in the two largest clusters in the right and left frontal lobes (p < 0.001).
Finally, the team reported other smaller clusters found in the basal ganglia, left occipital, and cerebellum (p < 0.001).
Satoh said these findings contribute to a greater understanding of the neuroinflammatory profile and the pathophysiological process of PAOS neurodegeneration.