Evidence supporting the clinical value of PET/MRI continues to mount, as a small study from Germany has found that the hybrid modality is effective for evaluating patients with large-vessel vasculitis (LVV).
One potential benefit is the lack of radiation exposure with contrast-enhanced MRI versus contrast-enhanced CT. MRI also delineates soft tissue better than CT, promoting greater accuracy in LVV assessment.
"PET/MRI potentially leads to a more precise evaluation of disease activity and extent of LVV compared to other modalities, which might influence further patient management," lead author Dr. Ingo Einspieler, a resident in the department of nuclear medicine at Technische Universität München (TUM), told AuntMinnie.com by email. "However, to prove that, a comparison with other modalities such as PET/CT is still needed."
PET has already proved beneficial for assessing inflammatory activity in large-vessel vasculitis and is routinely used in combination with CT. However, the shortfall is that CT does not offer the image quality or soft-tissue contrast of MRI.
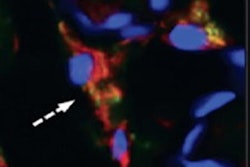
"Therefore, combined PET/MRI would offer not only sensitive evaluation of inflammatory processes in arterial vessels, but also detailed morphological analysis," Einspieler said. "This potentially enables exact coregistration of PET and MRI data and differential diagnosis to other inflammatory aortic diseases, like retroperitoneal fibrosis or inflammatory abdominal aortic aneurysm."
Pilot parameters
In the study, which was presented at the Society of Nuclear Medicine and Molecular Imaging (SNMMI) 2014 annual meeting, Einspieler and colleagues retrospectively reviewed results from 12 consecutive LVV patients seen between August 2011 and March 2014. The group consisted of 10 women and two men, with a mean age of 62.5 years (range, 27 to 80 years).
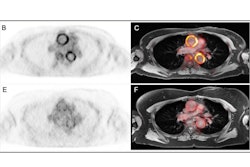
A total of 16 PET/MRI exams (Biograph mMR, Siemens Healthcare) were performed (four PET/MRI scans were for follow-up studies), along with 12 PET/CT exams using a low-dose technique. The researchers also enrolled a reference group of 16 patients, who were similar to the study group in terms of age, gender, PET/MRI acquisition time, and atherosclerosis risk factors, to determine cutoff values for pathological FDG uptake.
MR imaging sequences included T2-weighted short-tau inversion recovery (STIR) to explore edema in the vessel wall and wall diameter; T1-weighted volumetric interpolated breath-hold examination (VIBE) with and without contrast for wall diameter; and contrast-enhanced MR angiography for stenosis, occlusions, and aneurysms.
The patients fasted for at least six hours before FDG injection. PET/MRI scans started approximately 146 minutes (± 33 minutes) after administration of 328 MBq (± 60 MBq) FDG.
Image analysis
Three board-certified readers analyzed 10 vessel segments: both common carotid arteries, both subclavian arteries, the ascending aorta, the aortic arch, the descending thoracic aorta, the abdominal aorta, and both iliac arteries.
To quantify FDG vessel uptake, the researchers used a four-point rating system in which 0 indicated no FDG uptake, 1 meant low-grade FDG uptake (less than the liver), 2 was intermediate-grade FDG uptake (similar to liver), and 3 indicated high-grade FDG uptake (greater than that of the liver).
Cutoff values for pathological FDG vessel uptake in the 10 vessel segments were grade 3 in the common carotid arteries and either grade 2 or 3 in the other vessel segments.
The team also used PET to assess an additional nine vessel segments in the LVV group: both renal arteries, both femoral arteries, both vertebral arteries, the celiac trunk, the superior mesenteric artery, and the inferior mesenteric artery. Grade 3 uptake was defined as pathological in these nine vessel segments.
PET/MRI efficacy
In the review of images, PET showed high FDG vessel uptake suspicious for vasculitis in 15 (94%) of 16 exams. Grade 3 FDG vessel uptake was evident 13 cases, grade 2 uptake was seen in two cases, and grade 1 uptake was seen in one case.
MRI showed morphological changes associated with vasculitis in 12 (75%) of the 16 exams. Wall thickening was seen in 12 cases, followed by contrast-enhancement of the vessel wall in nine cases and STIR-signal elevation in the vessel wall in another nine cases.
PET/MRI uncovered active disease in 15 (94%) of the 16 examinations, according to the researchers.
In terms of disease extent, PET/MRI detected 95 vessel regions with functional and/or morphological changes associate with vasculitis.
PET showed 86 regions with pathological FDG vessel uptake suspicious for vasculitis, while MRI showed 49 vessel regions with morphological changes associated with vasculitis. PET was equal to MRI in 40 vessel regions, PET exceeded MRI for 46 regions, and MRI exceeded PET in nine regions.
Future studies
"Both PET and MRI can visualize disease activity and extent of LVV, with an advantage to PET regarding our results," Einspieler said. "However, only MRI can display potentially life-threatening late disease complications, such as vessel stenosis or occlusions, potentially leading to surgical intervention or angioplasty."
"According to our results, only the combination of PET and MRI seemed to demonstrate the whole disease extent of LVV, which could have an impact on further patient management," he added.
To what extent PET/MRI findings could direct patient treatment is the subject of a future trial.
"We definitely want to continue our research in LVV and plan to do a larger follow-up trial to prove the role of PET/MRI in therapy monitoring of LVV," Einspieler said. "In the future, it has to be evaluated if PET/MRI, which is substantially more expensive and complex, has an added benefit over PET/CT."