PET imaging with somatostatin receptor 2 (SST2) radiotracers shows major promise for diagnosis and therapeutic monitoring in patients with large-vessel vasculitis (LVV), according to a group in the U.K.
Researchers led by Dr. Andrej Corovic of the University of Cambridge showed for the first time in that SST2 receptors are expressed by inflammatory macrophages within inflamed arteries of patients and that this activity can be detected using PET/MRI imaging. The finding bodes well for eventual use of the tracers in clinical practice, they wrote.
"By repurposing existing PET tracers for this novel application, we describe a method that has the potential to be rapidly incorporated into clinical practice," the group noted. The study was published January 23 in the Journal of the American College of Cardiology.
LVV is a chronic relapsing systemic inflammatory disease that can lead to stroke and aortic aneurysms. It is the most common primary vasculitis in adults and is primarily treated with steroids to induce remission.
Assessing inflammatory disease activity in LVV can be challenging by conventional measures, according to the group. F-18 FDG PET imaging is typically used, yet it is limited by high false-positive rates among LVV patients in remission. Animal studies have shown that SST2 radiotracers may be more specific, detecting activated inflammatory macrophages in atherosclerotic plaque, the authors wrote.
Moreover, one of the tracers used in this study, gallium-68 (Ga-68) DOTATATE, has been shown to detect SST2 activity in neuroendocrine tumors, while the second, F-18 FET-bAG-TOCA, is being evaluated as a longer-lasting alternative to Ga-68 DOTATATE in separate research.
Corovic and colleagues tested the ability of these SST2-targeted tracers to characterize LVV disease activity via a study that included 61 participants who underwent SST2-PET/MRI imaging using an integrated scanner. Patients were divided into three groups: 27 with LVV, 25 with a recent atherosclerotic myocardial infarction, and nine controls who underwent imaging for an oncologic indication. Three rheumatologists graded clinical LVV status independent of the study findings as "active" (new diagnosis or acute flare), "grumbling" (low-grade residual arteritis), or "inactive" (disease in remission).
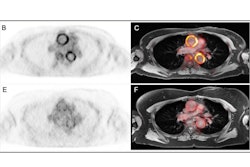
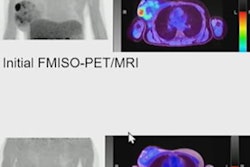
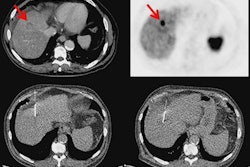
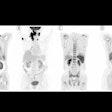
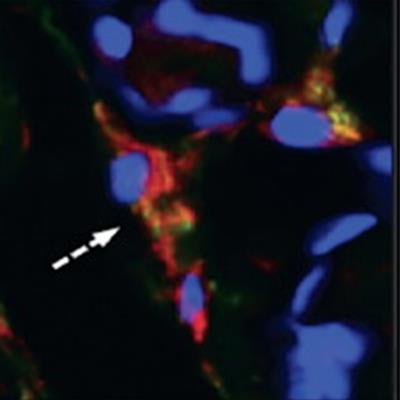
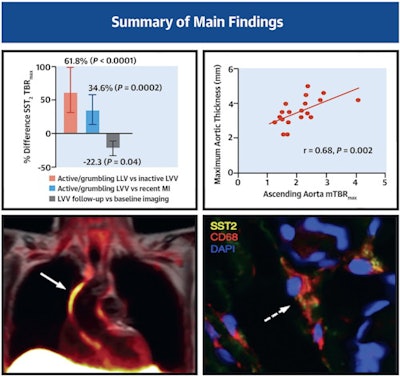 Patients with large vessel vasculitis (LVV) and recent atherosclerotic myocardial infarction (MI) underwent somatostatin receptor 2 (SST2) PET/MRI in a prospective observational cohort study. Arterial SST2 signal (arrow) measured by the maximum tissue-to-background ratio (TBRmax) using PET/MRI accurately differentiated patients with active/grumbling LVV from those with inactive LVV and recent MI, as well as control subjects. There was also a strong correlation between SST2 mean TBRmax and para-aortic thickening in LVV patients. SST2 expression was identified in macrophages (dashed arrow), pericytes, and perivascular adipocytes with arterial specimens from patients with LVV. Image courtesy of the Journal of the American College of Cardiology through CC BY 4.0.
Patients with large vessel vasculitis (LVV) and recent atherosclerotic myocardial infarction (MI) underwent somatostatin receptor 2 (SST2) PET/MRI in a prospective observational cohort study. Arterial SST2 signal (arrow) measured by the maximum tissue-to-background ratio (TBRmax) using PET/MRI accurately differentiated patients with active/grumbling LVV from those with inactive LVV and recent MI, as well as control subjects. There was also a strong correlation between SST2 mean TBRmax and para-aortic thickening in LVV patients. SST2 expression was identified in macrophages (dashed arrow), pericytes, and perivascular adipocytes with arterial specimens from patients with LVV. Image courtesy of the Journal of the American College of Cardiology through CC BY 4.0.The study found that radiotracer activity decreased significantly across groups of individuals with active, grumbling, and inactive LVV. Specifically, vessel SST2 maximum tissue-to-blood ratio was 61.8% higher in active/grumbling LVV than inactive LVV and 34.6% higher than in patients with myocardial infarctions, with good diagnostic accuracy (area under the curve [AUC] ≥ 0.86; p < 0.001 for both). Conversely, the SST2 signal was not elevated in any of the control subjects.
Furthermore, among a subgroup of 10 individuals with available F-18 FDG-PET/CT imaging, the uptake of the SST2-targeted tracers correlated visually with F-18 FDG uptake, the authors added.
"We show for the first time, to our knowledge, that SST2 receptors are expressed by inflammatory macrophages, as well as pericytes and perivascular adipocytes, within inflamed arteries of patients with LVV and can be detected using PET/MRI," Corovic and colleagues reported.
In an accompanying editorial, Dr. Ahmed Tawakol and Dr. Michael Osborne of Massachusetts General Hospital in Boston wrote that several key opportunities emerge from the study findings. First, SST2 imaging may fulfill an unmet need for a more specific PET tracer than F-18 FDG to help identify ongoing low-level LVV activity, and second, it's possible that SST2-targeted tracers would be useful for evaluating novel therapies for LVV and for other conditions in which inflammation plays an important role, such as atherosclerotic disease.
"Because SST2-targeted radiotracers are already implemented clinically for other indications, the current findings could have substantial implications for the care of patients with LVV and, potentially, other inflammatory conditions in the relatively near future," Tawakol and Osborne concluded.