
If you’re planning to snowboard or skate competitively, chances are you’ll injure your wrist sometime during your career. After all, failure is part of learning, and in these sports when you fail you fall. And when you fall, more likely than not you’ll use your hands and wrists to cushion the impact (American Journal of Sports Medicine, September-October 2001, Vol. 29:5, pp. 581-585).
According to a study by Dr. Martin Mack and colleagues at the Johann Wolfgang Goethe-Universtät in Frankfurt/Main, Germany, high-resolution MRI has advantages over conventional film-screen radiographs in the early diagnosis of wrist trauma.
"The problem with conventional radiographs of wrist trauma is that they often cannot clearly depict bony fractures," said Mack in a presentation at the 2001 RSNA meeting. "We evaluated the clinical impact of MR imaging in wrist trauma diagnosis and documented the influence it had on the period of sickness and being unfit for work."
The group performed the scans on a 1.5-tesla unit (Symphony Quantum, Siemens Medical Solutions, Iselin, NJ), obtaining coronal and axial T1-weighted images and coronal T2-weighted sequences, using STIR (short-tau inversion recovery), and a dedicated small-extremity flex coil.
"The TI SE sequence for the transversal and coronal views used a TR/TE of 548/18, a slice thickness of 2 mm, a 512 x 512 matrix, a FOV of 80-120 mm, and an exam time of 3 minutes, 41 seconds. The T2-STIR for the coronal views used a TR/TE of 4,650/70, a 2 mm slice thickness, a 256 x 256 matrix, a FOV of 80-120 mm, and a time of 4 minutes, 36 seconds," noted Mack.
The study group consisted of 36 men and 18 women with a mean age of 36.1 years. Their inclusion in the study was on the basis of three factors:
- Acute wrist trauma.
- Pain.
- No definite fracture on conventional radiographs and special scaphoid radiographs.
Based on plain-film results, there was clinical suspicion of wrist fractures in 21 patients, with the remaining 35 patients’ radiographs labeled as indistinct. The patients all exhibited pain on palpation of the fovea radialis, or at the dorsal hand or forearm. There was constant pain with or without stress reported by the patients, as well as limited movement out of pronation, or in dorsal flexion or extension.
Radiographs were acquired at a mean of 1.6 days following the wrist trauma. MR imaging was performed within a mean of 6.6 days after the initial radiographs. The initial radiographs were then evaluated by two senior radiologists who were unaware of the MRI findings. They diagnosed no fractures on 20 and 28 of the patients, respectively, from the radiographs.
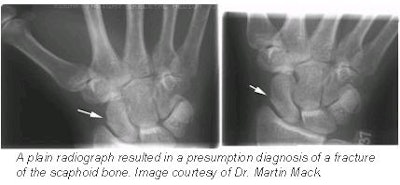 |
The same evaluation team then reviewed the MRI results and found scaphoid, radius, and other fractures in 20 of the patients, with 36 showing no fracture. There were false-positive results on plain radiographs in more than half of the patients. False-negative diagnoses of the radiographs were found in 6 cases. Between MRI and the radiographs, the diagnostic agreement of the observers was 44.6% and 55.4%, respectively.
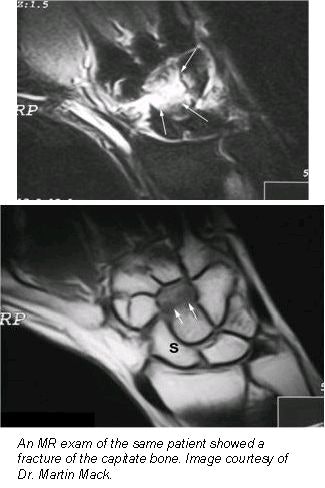 |
In more than a third of the patients, MRI allowed for the detection of additional injuries to soft tissue. Bone bruises were found on 15 patients, discus lesions were observed in 7, and ligament injuries and ligament avulsion were found in 5 and 8 patients, respectively. In addition, 13 patients were diagnosed with joint effusion, and cysts were discovered in 3 patients.
For Mack and colleagues, the therapeutic consequences of using MRI in wrist trauma was undeniable. MRI changed the therapy in 62.5% of patients in the study group. For 3 patients, MRI preceded surgery, while for 22 patients, the immobilization period was shortened. And for 12 patients, MRI resulted in a prolonged immobilization.
From an economic standpoint, early use of MRI for wrist trauma was compelling, Mack said. MRI influenced recovery time in 23 of 54 patients. In 15 of these 23 patients, MRI shortened recovery time, saving 59 total workweeks. In the remaining 8 patients, MRI resulted in a longer recovery time, for a loss of 37 total workweeks.
"Complete high-resolution MR workup of the acute wrist trauma can be performed in eight minutes' scan time using only T1-weighted and fat-saturated T2-weighted sequences in coronal slice orientation. Axial images were not helpful regarding the diagnostic accuracy," Mack said.
The team advocates that clinicians perform MRI of the wrist as soon as possible after trauma if there is any clinical indication of injury, and radiographs are normal. The results show that MRI offers an accurate diagnosis in less than 10 minutes, and may reduce economic costs due to shortened immobilization time in cases with a suspected fracture on plain radiographs.
"On the basis of our research, I also recommend early MRI of the wrist in acute trauma in patients with clinical suspicion of a lesion and normal plain radiographs who have incurred the trauma as the result of a sports injury," Mack told AuntMinnie.com.
By Jonathan S. BatchelorAuntMinnie.com staff writer
February 10, 2002
Related Reading
UK's junior doctors frequently misdiagnose wrist injuries, January 11, 2002
Extremity MRI improves early evaluation of rheumatoid arthritis, August 20, 2001
Magnetic Resonance Imaging in Orthopaedics & Sports Medicine, May 22, 2001
MRI detects synovitis of hand, wrist joints in rheumatoid arthritis, February 19, 2001
Copyright © 2002 AuntMinnie.com




















