Whole-body MRI performed with a rolling-table platform may prove valuable in tumor staging, according to a study published in this month's American Journal of Roentgenology. Preliminary research from the University Hospital Essen in Germany concluded that 3-D volumetric interpolated whole-body MRI could be a potential alternative to conventional multimodality tumor-staging strategies.
Whole-body MRI has been discussed previously as a generalized tumor-staging tool, but long examination times, limited spatial resolution, and the presence of imaging artifacts have limited the procedure, the German researchers said. But a volumetric interpolated breath-hold examination -- in the form of a fat-saturated, 3-D gradient-echo sequence with nearly isotropic resolution -- may overcome the technique's shortcomings.
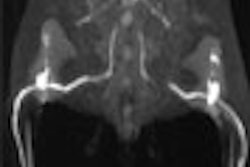
To expand the utility of the MR sequence beyond a single anatomic region, the researchers deployed a rolling-table platform with integrated surface coils for whole-body MR angiography (AngioSurf, MR Innovation, Essen, Germany). The rolling-table platform requires a scanning time averaging 11 minutes.
The group studied four males and four females in July and August 2001. Imaging was performed on a Magnetom Sonata 1.5-tesla system (Siemens Medical Solutions, Erlangen, Germany), equipped with high-performance gradient systems offering a maximal gradient amplitude of 40 mT/m and a slew rate of 200 mT/m/msec, according to the authors (AJR, August 2002, Vol. 179:2, pp. 445-449).
Based on 3-D spoiled gradient-echo acquisition, the volumetric interpolated breath-hold examination includes a TR/TE of 3.1/1.2 msec, a flip angle of 12 degrees, and a bandwidth of 490 Hz/pixel. The researchers used a slab thickness of 312 mm for all measurements. They obtained 65 partitions, which were subsequently interpolated to 104 partitions for a final slice thickness of 3 mm.
A rectangular field of view of 350 x 219 mm2 and a data acquisition matrix of 120 x 256 data points resulted in an in-plane resolution of 1.8 x 1.4 mm2, which was interpolated by zero filling to a matrix of 240 x 512 for a final pixel size of 0.9 x 0.7 mm2, the group stated. Data acquisition time for a 3-D volume was 22 seconds. The 3-D sequence incorporates a frequency-selective fat-saturation pulse before each partition loop, which is centrically recorded to maximize fat saturation, the researchers wrote.
All patients also underwent thoracic, abdominal, and pelvic helical CT studies. Contrast-enhanced helical CT was performed in three patients to exclude brain metastases. Five patients received skeletal scintigraphy procedures. All examinations were performed 3-13 days before the whole-body MR examination, with an average of 7.6 days, according to the researchers.
Two radiologists interactively analyzed the 3-D MR imaging data sets of each whole-body examination on Siemens' Virtuoso workstation using its multiplanar reformation mode. Discrepancies were resolved by consensus.
The reviewers were not informed about the results of other imaging studies, although they were provided with information on patient age, sex, and primary tumor. The radiologists evaluated the images for the presence of metastatic disease, and numerically quantified metastases for lung, liver, bones, and other anatomic regions such as the cerebrum, retroperitoneum, and skin.
For each anatomic region, the diameter of the smallest metastasis detected on whole-body MR imaging was also measured, and the whole-body MR findings were directly compared with the reference examinations to assess agreement, according to the study team.
Whole-body MR imaging detected hepatic metastases in six patients, and more than five hepatic metastases were identified in three patients. The smallest hepatic metastasis measured 6 mm in diameter, according to the researchers.
The MR study produced no false-negative findings and detected pulmonary metastases in five patients. In one patient, however, a lung metastasis (5 mm in diameter) on CT was missed on MR imaging, the researchers reported.
The smallest pulmonary metastasis measured 8 mm in diameter. In addition, MR imaging revealed retroperitoneal metastases in one patient with testicular cancer and a metastasis in the dorsal abdominal wall in another patient; both findings were confirmed on CT.
Bone metastases evidenced by increased signal intensity on contrast-enhanced volumetric interpolated breath-hold images were detected on MR imaging in four patients. These metastases were found in the spine in three patients, the pelvis in three patients, and the ribs in two patients.
Osseous metastases were visualized in the scapula and the femur in two patients. MRI findings had good correlation with bone scintigraphy except in one patient. In that case, MRI showed osseous lesions in the lumbar spine, whereas skeletal scintigraphy did not, the researchers wrote. The presence of bone metastasis was eventually confirmed at biopsy. All other MR findings regarding osseous metastases were confirmed on skeletal scintigraphy.
As for cerebral metastases, MRI detected metastases ranging between 8-15 mm in diameter in two patients. All metastases, and their absence in a third patient, were confirmed on CT, the researchers found.
"Certainly, whole-body MR imaging will not replace dedicated MR examinations, which can exploit a host of different contrast mechanisms for the study of individual organ systems," the authors wrote. "The aim of the described strategy is focused solely on the detection and follow-up of metastatic lesions in patients with known primary tumors. If identified lesions cannot be reliably characterized as metastatic, additional examinations are required."
The researchers are hopeful that their work will motivate others to evaluate the clinical potential of whole-body MR imaging in larger patient cohorts.
By Erik L. RidleyAuntMinnie.com staff writer
August 28, 2002
Related Reading
Multi-organ MRI/MRA screening finds unsuspected pathology, April 18, 2002
AngioSURF rides new wave in MR angiography, April 11, 2001
Copyright © 2002 AuntMinnie.com



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)

.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)