Real-time MRI combined with dobutamine hydrochloride stress can reliably detect ventricular wall-motion abnormalities (WMA), according to researchers at the German Heart Institute in Berlin.
Writing in the September issue of Radiology, Drs. Simon Schalla, Christoph Klein, Ingo Paetsch and colleagues compared the real-time technique with standard echo-planar MR imaging, and with coronary angiography in 22 patients with known coronary artery disease. The group concluded that real-time MR allows accurate detection of WMA under stress conditions. (Radiology, September 2002, Vol. 224:3, pp. 845-851).
Dobutamine hydrochloride-induced stress ECG is a widely used pharmacologic stress-inducing agent, which enables the detection of myocardial ischemia by visualizing WMA, the authors wrote. However, image quality is a limiting factor in 10-15% of ECG exams. And while standard echo-planar MR with dobutamine is more accurate than ECG with dobutamine in many patients, traditional MR suffers from limitations due to its long acquisition times (10-16 seconds) acquired over several heartbeats, and long reconstruction times.
Complete real-time cardiac images are now possible due to the development of high-performance gradients and hybrid sequences that combine turbo gradient-echo and echo-planar MR imaging. And although spatial resolution is reduced in real-time imaging, the technique has been reported to sufficient for detecting WMA.
"This technique has several advantages when compared to conventional acquisition techniques because the complete data set is acquired during a single measurement interval and not during several heartbeats," they wrote. "Breath holding is not necessary to preserve image quality, and although ECG monitoring is important for the patient's safety, it is no longer required to trigger imaging." The technique could potentially be applied to ergometric stress testing as well, they wrote.
The study included 22 patients (19 men and 3 women, mean age 64) with known CAD who were scheduled to undergo coronary angiography. Dobutamine hydrochloride (280 mg/50 ml) was infused intravenously over 3 minutes at 10, 20, 30 and 40 micrograms per kg of body weight, and the highest dose was supplemented with 0.25 fractions of atropin sulfate until patients had reached 85% of their age-predicted heart rate.
Images were acquired in the supine position using a Gyroscan ACS-NT scanner (Philips Medical Systems, Best, the Netherlands) using Cardiac Patch CPR6 research software, rapid gradient systems (21 mT/m amplitude, 100 mT/m/sec slew rate), and a five-element phased-array cardiac coil. Only two elements were used to avoid aliasing the small field of view.
Survey images were acquired, followed by three short-axis sections using a segmented k-space echo-planar stress-imaging sequence as a reference standard. Then, using identical section positions, real-time sequences were acquired using a hybrid segmented k-space turbo gradient-echo echo-planar imaging sequence with a repetition time msec/echo time msec of 16.5/6.8, and spatial resolution of 2.2 x 4.4 mm. Thirty images were acquired to cover two cardiac cycles.
Continuous cine loops were assessed visually to perform qualitative MR image analysis. The readers examined image quality, endocardial movement, and systolic wall thickening during stress, and compared them with images acquired at rest. The left ventricular myocardium was divided into 16 segments, with each assessed for wall motion at rest, at medium and maximum stress. Wall motion was deemed abnormal if hypokinesia, akinesia or dyskinesia was observed.
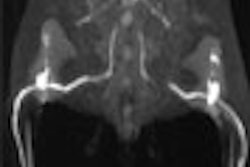
Following both types of MR imaging, the group performed biplanar coronary angiography on all patients using multiple projections. The results were evaluated qualitatively, and quantitatively when the examiner had any doubt about the findings.
The age-predicted heart rate was reached using dobutamine chloride (mean dose: 39 ± 4.30 μg/kg body weight plus 0.31 mg) without any apparent adverse effects, the authors wrote. Compared with echo planar imaging, real-time MR's k values for detecting wall motion abnormalities were .97 at rest, and .94 at maximum dobutamine chloride stress.
Compared with angiography, real-time MR imaging had sensitivity of 81% (13/16 patients) and specificity of 83% (5/6 patients) for detecting significant coronary arterial stenosis. Echo-planar MRI had sensitivity of 88% (14/16 patients) and specificity of 83% (5/6 patients) compared with angiography.
Real-time image acquisition is similar to echo-planar imaging for the detection of WMAs in patients with coronary artery disease, the authors concluded, and the contrast between blood and myocardium sufficient to adequately assess wall motion WMAs.
"In contrast with conventional MR imaging techniques...ECG triggering is not necessary to preserve image quality, and high-quality images can be obtained even in patients with arrhythmia. Patients with atrial fibrillation, frequent premature heartbeats, or sinus arrythmia may have moderately reduced image quality" with conventional MR techniques, they wrote. But acquiring images in real time (65 msec) eliminates the effect of these pitfalls on image quality. Moreover, the ability to image the entire heart in 12-16 seconds may further improve the accuracy of the technique compared with conventional MR, they wrote.
Study limitations included the acquisition of images at just two stress levels due to patient safety considerations, as well as the small and inhomogeneous study population, nearly all of whom had a previous myocardial infarction, with most having undergone revascularization procedures. And reconstruction had to be performed offline due to software limitations, precluding online monitoring of new WMAs.
The major technical limitation was low spatial resolution: 2.2 x 4.4 mm for real-time MR vs. 1.3 x 2.6 mm for echo-planar, the authors wrote.
"This spatial resolution is probably not sufficient for detecting viable myocardium," they stated," since a dobutamine hydrochloride-induced increase in 2-mm or greater wall thickening is regarded as a diagnostic criterion for myocardial viability. However, for visual detection of WMAs, spatial resolution was sufficient, probably because of the eye's ability to interpret motion patterns rather than thickness alone."
By Eric BarnesAuntMinnie.com staff writer
September 23, 2002
Related Reading
Late-enhancement MRI compares to FDG-PET for gauging myocardial viability, August 26, 2002
Multi-organ MRI/MRA screening finds unsuspected pathology, April 18, 2002
Monitoring cardiac sarcoidosis with MRI could save lives, April 1, 2002
Copyright © 2002 AuntMinnie.com