NEW ORLEANS - Phosphorus (31P) magnetic resonance spectroscopy (MRS) can identify neuroischemic changes in the diabetic foot, according to a report Sunday at the American Diabetes Association meeting.
"Currently there are no satisfactory noninvasive methods to evaluate vascular tissue of the lower extremity in diabetic patients," explained lead author Dr. Lalita Khaodhiar from Beth Israel Medical Center and Harvard Medical School in Boston. "Phosphorus MRS noninvasively measures altered metabolic indices of muscle tissue in diabetes; however the technique has poor resolution and is time-consuming."
Recently, 31P data have been acquired directly into an image format using a technique known as rapid acquisition with relaxation enhancement (RARE) that yields higher spatial and temporal resolution than MRS.
The study population consisted of 10 patients with diabetic neuropathy and 11 healthy subjects. The group compared high-resolution MRI images for blood flow to phosphorus images for metabolic activity. They also assessed the relationship between changes in muscle blood flow and metabolism, and changes in the vascular reactivity of the microcirculation.
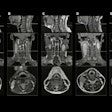
Scans were performed on a 3-tesla MR scanner to acquire standard T2-weighted MR transaxial images of the foot. RARE 31P scans were then obtained in the same plane. Phosphorous concentrations were estimated by comparing the ratio of the reference standard image signal to the highest-intensity signal in the muscle images.
The spatial distribution of the 31P image intensity was also compared to the spatial distribution of image intensity of the T2-weighted images. Laser Doppler perfusion imaging was used to measure the vascular reactivity at the dorsum of the foot.
Khaodhiar reported that the 31P intensity in normal subjects was uniform across the entire area of muscle. In the patients with diabetic nephropathy, there was a substantial variation with focal areas of undetectable 31P signal.
Comparison with T2-weighted images revealed low 31P signal regions corresponding to bright regions in the T2-weighted images, which indicates areas where the T2 parameter has been lengthened due to pathology, she said.
The total 31P intensity in the images was reduced in the diabetic neuropathy group compared to controls (1.3 ± 2.0 versus 4.2 ± 1.5, p = 0.001).
The total 31P intensity correlated with age, Neuropathy Disability Scale (NDS), and the endothelium dependent and independent vasodilatory responses in the microcirculation.
"Our results show that 31P RARE imaging can be used to distinguish healthy normal muscle from ischemic or diseased muscle, enabling the identification of focal areas of diseased and healthy tissue," Khaodhiar said. This noninvasive technique may provide essential information for determining interventional strategies and monitoring the progress of therapy in patients, she added.
By Jill SteinAuntMinnie.com contributing writer
June 16, 2003
Related Reading
Dobutamine stress echo aids prediction of CAD events and death in diabetics, April 9, 2003
Islet cell transplantation may replace insulin for diabetes, March 31, 2003
Calcified plaque increased in coronary arteries of diabetics, March 20, 2003
Undiagnosed diabetes common in patients scheduled for coronary angiography, March 4, 2003
Copyright © 2003 AuntMinnie.com


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)





.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)