For patients with connective tissue disorders such as Marfan syndrome or systemic lupus erythematosus (SLE), aortic root dilatation can be a leading cause of morbidity and mortality. In terms of imaging these patients, 2-D transthoracic echocardiography (TTE) has been the gold standard for determining if patients are at high risk for developing annuloaortic ectasia, according to Dr. Alan Stolpen, Ph.D., from the University of Iowa in Iowa City.
The Holy Grail of TTE was set out in a 1989 article by a group from New York Hospital-Cornell Medical Center in New York City, Stolpen explained during a presentation at the 2003 RSNA meeting in Chicago. They wrote that "aortic root dilatation is currently detected by nomograms based on M-mode echocardiographic data." Aortic root diameters are measured by TTE at the sinuses of Valsalva, supra-aortic ridge and proximal ascending aorta. These measurements are compared with age, gender, body habitus, blood pressure and stroke volume, and with M-mode findings and normal limits (American Journal of Cardiology, September 1989, Vol. 64:8, pp. 507-512).
But TTE does have its drawbacks, including an acoustic window requirement, which can limit application in some patients; blind spots such that the entire aorta isn’t always visualized; and limited capabilities in patients with Marfan syndrome, said Stolpen, who is an associate professor of radiology, and co-director of MRI at the university.
"MR, which is a well-established modality for studying the aorta, offers a potentially more robust alternative or complement to TTE," Stolpen said. "The purpose of our study was...to assess the agreement between MRI and TTE for aortic root measurements (and) to compare the robustness. By that I mean, how often was the image quality sufficiently good to enable four-point measurements?"
For this retrospective study, Stolpen and colleagues looked at 59 consecutive patients who underwent cine MRI with TTE correlation from September 2000 to April 2003. The patients had a diagnosis, or strong family history, of Marfan syndrome, Ehlers-Danlos syndrome, familial thoracic aortic aneurysm syndrome, or a bicuspid aortic valve.
"In Marfan patients, the scoliosis and pectus deformity can displace the heart to the left, which makes it very difficult for TTE to select the correct imaging," Stolpen wrote in an e-mail to AuntMinnie.com. "Also, TTE image quality in these patients tends to be poor."
MR studies were performed on a 1.5-tesla scanner (Signa CV/i, GE Healthcare, Waukesha, WI) using a breathhold-segmented k-space cine 2-D FIESTA protocol or a fast GRE protocol. The mean time between MRI and TTE was 118 days.
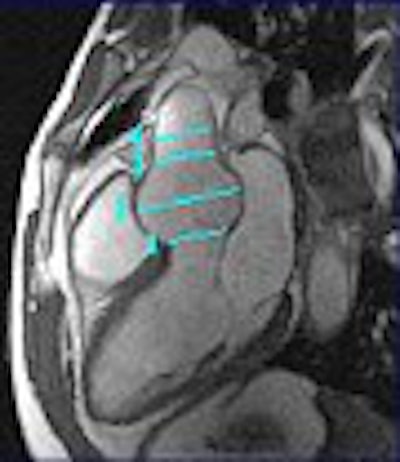
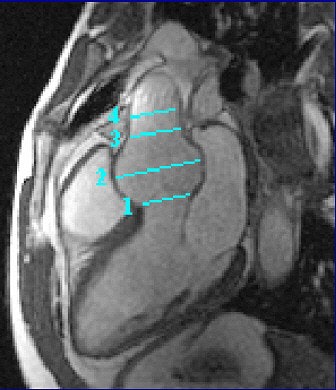 |
| Two-dimensional, steady state free precession cine MRI acquired during diastole, including the four locations for aortic root measurements. Image and caption courtesy of Dr. Alan Stolpen, Ph.D. |
For both modalities, the aortic root was imaged in the parasternal long-axis plane. Standard measurements were obtained at the aortic annulus, sinuses of Valsalva, sinotubular junction, and proximal ascending aorta. The Bland-Altman analysis was used to assess agreement between TTE and MRI.
According to the results, out of 252 possible measurements (four sites in 63 exams), cine MRI failed to provide four measurements. In comparison, TTE failed to provide 24. In 18% of the TTE, the exam was inadequate because of technical difficulties or a poor acoustic window, Stolpen said.
The mean difference between MRI and TTE, and the standard deviation, was 0.04 ± 0.45 cm at the annulus in 57 cases; 0.01 ± 0.32 cm at the sinuses in 62 cases; -0.41 ± 0.50 cm at the sinotubular junction (59 instances); and 0.35 ± 0.57 cm at the proximal ascending aorta. Thirty-eight percent of the TTE exams failed to obtain measurements, compared to 7% of the MR exams.
However, "there was modest negative bias for MR at the sinotubular junction, and a similar negative bias at the proximal aorta. The problem has to do with the standard deviation, which was large across the board (up to 18% of the aortic diameter). The problem is that there was considerable variability in agreement between (the modalities) of the aortic root location," Stolpen said.
In his e-mail, Stolpen elaborated on the reasons for the negative bias.
"There are many reasons why MR and (TTE) aortic root measurements could differ. Most have to do with incorrect positioning of the imaging plane," he wrote. "For TTE, the parasternal long-axis view is one of the many long-axis views through the left ventricle. I think this view shows the aortic valve annulus and sinus very well, but the sinotubular junction and proximal aorta can be more difficult to see, and the latter may be in a slightly different imaging plane." In addition, there is no exact location for the proximal ascending aorta. As a result, TTE makes the measurement as far from the sinotubular junction as possible, which may not be far enough, he added.
However, with MR it is possible to see the entire ascending aorta, and most likely a more distal measurement was obtained, Stolpen explained. But in an effort to capture the parasternal long axis, and optimally depict all four aortic root locations as well as the mitral valve, an MR image may require the sacrifice of the left ventricular (LV) apex, particularly if it isn’t in the plane.
"Why should it matter if the measurements are different? Because the decision to intervene surgically is based on aortic root size and, to a lesser extent, on the rate of increase (and degree of aortic insufficiency). So differences between echo and MR could lead to inappropriate clinical management," Stolpen said.
While cine MRI did prove to be the better imaging modality in this study, Stolpen cautioned that MR and TTE might not be perfectly interchangeable for measuring aortic root dimensions. At his institution, TTE is still routinely performed, with MR reserved for adjunct imaging.
"Besides robustness, the real question is which modality provides more reproducible measurements," Stolpen said. "(That) study hasn't been done yet, but our preliminary data indicates high variability for echo (which contradicts the echo literature), and lesser variability for MR."
Also in MR’s favor: Pediatric and adult cardiologists at his institution, who routinely see patients with connective tissue disorders, have come to value the reliability and robustness of MR, according to Stolpen.
"(They) will make clinical decisions based on MR, even when results disagree with TTE," he said.
By Shalmali PalAuntMinnie.com staff writer
March 1, 2004
Related Reading
Active bone formation may cause aortic valve stenosis, May 6, 2003
Transesophageal MRI improves evaluation of aortic plaque, April 4, 2003
MRI links carotid artery plaque inflammation to unstable angina, March 10, 2003
Copyright © 2004 AuntMinnie.com



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











