
Botulinum toxin, commonly known as Botox, is used for blocking muscle spasms, barring excessive sweat, and, of course, banishing wrinkles. Now a multidisciplinary group in Belgium has found that botulinum toxin can boost cancer treatment by opening up a tumor's vascular bed, making it more receptive to radiation and chemotherapy.
"There is a real need for developing ways of transiently opening the tumor vascular bed to alleviate tumor hypoxia and increase the efficacy of anticancer cytoxic therapies," explained Bernard Gallez, Ph.D., and colleagues in a Clinical Cancer Research paper. "The goal of 'provascular' (treatment) approaches is to increase tumor perfusion and oxygenation.... Radiotherapy could benefit from tumor reoxygenation because oxygen is a key factor in the response to irradiation" (February 15, 2006, Vol. 12:4, pp. 1276-1283).
The group updated the results of their animal studies in two poster presentations at the 2006 International Society for Magnetic Resonance in Medicine (ISMRM) meeting in Seattle. Gallez is from the Laboratory of Biomedical Magnetic Resonance at the Université Catholique de Louvain in Brussels. His co-researchers are from the departments of medical chemistry and radiopharmacy, molecular imaging, and pharmacology.
In the first experiment, fibrosarcoma and liver tumor models were implanted into the thighs of mice. The botulinum toxin (BoNT-A) solution in saline or saline solution alone were injected when the tumors reached a diameter of 6.7 mm. Local irradiation was performed with 20 Gy of 250-kVp x-ray in the tumor-bearing leg, three days after Botox injection. BoNT-A-treated mice also received a single dose of cyclophosphamide.
 |
| Typical MR perfusion images of FSa II fibrosarcoma tumors, three days after treatment. |
Anatomic landmarks were established with a multislice, T2-weighted spin-echo MR sequence. Single-slice, dynamic, contrast-enhanced 4.7-tesla MRI was used to monitor perfusion on the third day after BoNT-A or saline injection. A charcoal probe (electron paramagnetic resonance or EPR oximetry) was used to evaluate tumor oxygenation.
According to the results, the partial pressure of oxygen (p02), which was very low in the tumors before treatment, significantly increased after Botox administration and reached its maximal level after three days (3.2 mm Hg to 8.2 mm Hg). Based on MR perfusion and permeability maps, the fraction of pixels perfused by the MR contrast was greater for the BoNT-A tumors than for the controls (69.2% versus 39.9%, p < 0.05). "These results indicate that there are more areas of the tumor that are perfused after BoNT-A treatment with no changes in hemodynamic variables," the authors wrote.
With regard to radiation treatment, they found that tumors that were irradiated but did not receive Botox had a tumor regrowth delay of 11 days. Pretreatment with BoNT-A led to a significant increase in tumor regrowth delay (15.7 days), the group stated, adding that BoNT-A "radiosensitizes tumors through changes in the tumor microenvironment rather than by a direct sensitizing effect."
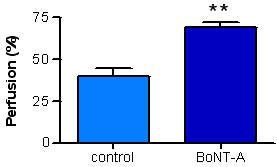 |
| Mean percentage of perfused pixels for treated and control groups. |
Gallez's group stressed the major findings of this study, all of which led to a substantial improvement in therapeutic response:
- Local administration of BoNT-A promotes tumor perfusion and oxygenation.
- BoNT-A interferes with vessel vasoreactivity.
- BoNT-A can increase the effectiveness of radiotherapy and chemotherapy.
In one ISMRM poster presentation, EPR oximetry was used to monitor p02 in vivo over a four-day period in mouse tumors injected with Botox. MRI was used to measure tumor perfusion. Once again, the authors found that the local administration of BoNT-A increased tumor oxygenation as well as perfusion, leading to a substantially better response to therapy.
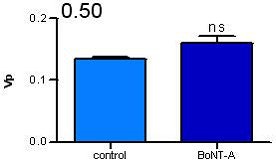
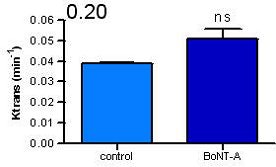
 |
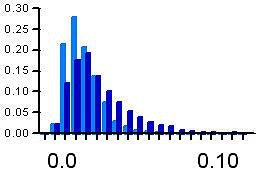 |
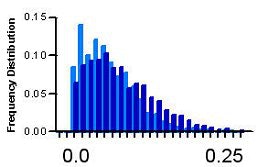
| Distribution of pharmacokinetics parameters in treated tumors. |
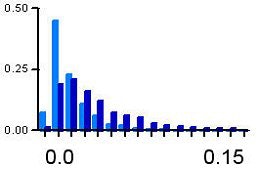 |
In the second ISMRM poster, the authors switched to 19F-MR spectroscopy (FMRS) and proton MRS to noninvasively study the kinetics of fluorinated chemotherapy agents in Botox-enhanced tumors. Tumors were implanted in 16 mice that were then injected with BoNT-A or a saline solution. FMRS was done on the same 4.7-tesla scanner with a 25-mm diameter surface coil. This coil was placed directly over the tumor to maximize the nuclear magnetic resonance (NMR) signal from the tumor and minimize the signal from the upper leg and paw.
They determined that the initial uptake of the chemotherapy agent (gemcitabine) in the Botox-treated tumors was about 40% higher than in the controls. "This supports our second hypothesis that BoNT-A should chemosensitize tumors to gemcitabine. Definitive experiments to test this latter hypothesis are under way," the authors stated.
 |
 |
| Overall estimation of pharmacokinetic parameters after BoNT-A treatment. All images courtesy of Bernard Gallez, Ph.D. |
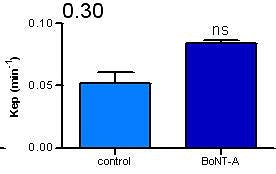 |
In an e-mail interview with AuntMinnie.com, Gallez discussed some of the details of his group's work as well as their plans for future research.
AuntMinnie: What was the impetus for this work and how did your group decide to test BoNT-A in this setting? Was the availability of Botox a factor?
We are working on the factors of the tumor microenvironment that favor response to anticancer treatments. Particularly, we are looking for treatments that can modulate tumor oxygenation and tumor perfusion in order to improve the response to radiotherapy and chemotherapy.
Concerning BoNT-A, we made the hypothesis that this toxin could interfere not only with the spasms of (skeletal) muscles, but also with the neurogenic tone in tumor vessels. Using EPR oximetry and (dynamic contrast-enhanced) MRI, it was possible to monitor changes in tumor microenvironment, and finally we applied therapy at the time of maximal reoxygenation and reperfusion of the tumors. The choice of BoNT-A was considered as it was already used in the clinic for the treatment of spasms, with local administration allowing the absence of systemic side effects.
You used MRI to study tumor perfusion and MRS to study the kinetics of the chemotherapy agents. Can these imaging tests be performed at the same time?
(In our studies) the measurements have been carried out on different series of animals. Concerning dynamic contrast-enhanced MRI and FMRS, it is indeed feasible to carry out the study at the same time.
What will be the next phase in your research? You mentioned in the Clinical Cancer Research paper that BoNT-A has a "long-term established absence of toxicity ... when used appropriately." Do you plan to conduct additional animal studies with follow-up to determine if there are negative effects from the Botox?
Classically, several normal tissue models are used to determine whether an agent is responsible for toxicity on early-responding tissue (e.g., intestinal regenerated crypt assay) or late-responding tissues (e.g., leg contracture assay).
However, in the case of BoNT-A, these assays are unnecessary as BoNT-A is administered directly inside the tumor with a very limited diffusion in the surrounding normal tissues. Even in this case, a radiosensitizing property on the normal tissue is unlikely as we showed that BoNT-A acts via an oxygen effect. Consequently, the radiosensitizing property will more than likely be higher for hypoxic tumor regions than for well-oxygenated tissues.
We discussed this issue with radiotherapists who found these preclinical toxicity studies were not really necessary.
Do you anticipate conducting tests in human subjects in the near future?
Some of our preclinical studies are discussed in our institution for possible clinical application and BoNT-A is one of the candidates. Before establishing its relevance in terms of therapeutic efficacy and tolerance, we first plan to establish the changes in the tumor microenvironment by imaging modalities. If results are comparable to animal studies, then it will be worthwhile to try the treatments for therapeutic relevance.
By Shalmali Pal
AuntMinnie.com staff writer
May 18, 2006
Botox image courtesy of Allergan.
Related Reading
Minimally invasive sympathectomy procedure cures palmar hyperhidrosis, December 1, 2005
Endoscope guides precise Botox delivery for anal fissure treatment, June 18, 2003
Copyright © 2006 AuntMinnie.com



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











