In one of the largest prospective clinical trials to date, researchers at the University of Michigan in Ann Arbor have found that functional diffusion-mapping MRI can provide an earlier assessment of response to radiation therapy treatment for glioma patients than traditional MRI. The researchers presented the study at the 2008 American Association for Cancer Research (AACR) meeting in San Diego.
Glioma is a notoriously hard-to-treat cancer of the central nervous system, primarily the brain. In their study, the researchers evaluated treatment response in 60 patients with glioma who underwent radiation therapy, sometimes accompanied by chemotherapy. Researchers found measurable changes in tumors using functional diffusion mapping one week after initiating therapy.
"At three weeks, functional diffusion mapping was a strong predictor of survival at one year," said lead researcher Brian Ross, Ph.D., a professor of radiology and biological chemistry at the University of Michigan Medical School and co-director of the molecular imaging program at the University of Michigan Comprehensive Cancer Center in Ann Arbor. The strongest predictor of survival was the use of functional diffusion mapping and conventional MRI together at 10 weeks, he added.
Ross said the trial suggested that functional diffusion mapping could be used to individualize treatment for glioma patients, and intervene early on in the course of treatment with more effective therapies.
"With functional diffusion mapping, you could potentially make decisions about treatment much earlier -- you could continue the treatment plan if it is working, or if not, could retarget regions of the tumor that are not dying," he said.
If the treatment is not working, doctors could potentially switch treatments much earlier than is done when tumor treatment response is measured by conventional MRI, Ross noted.
Patients with high-grade gliomas -- the type analyzed in the study -- have a high mortality rate, and people survive only an average of 12 months after diagnosis. Typically, patients receive six to seven weeks of treatment, followed by a traditional MRI scan several weeks after completing treatment to determine if the tumor shrank.
In the study, patients were assessed with functional diffusion mapping by diffusion MRI and standard MRI at one week, three weeks, and 10 weeks after starting radiotherapy. At 10 weeks, all the patients had completed their treatments.
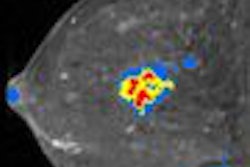
Although diffusion MRI did not produce a better quality image of the tumor, it was able to assess the response of the tumor to therapy at three weeks, while conventional MRI did not. At 10 weeks, the ability of standard MRI to predict survival and outcome was as accurate as functional diffusion mapping by diffusion MRI.
Ross noted that diffusion MRI is more accurate earlier in treatment because tumors may appear larger or have more contrast enhancement in response to therapy, even though they are not actually growing. "Diffusion MRI may help differentiate which patients are actually doing well," he said.
Diffusion MRI can be performed on any MRI system and measures the movement of water within body tissue. It's commonly used to evaluate brain injury in stroke patients, and is gaining popularity as an aid in diagnosing and evaluating cancer treatment.
Diffusion MRI enables clinicians to see the movement of water almost immediately, rather than waiting eight to 10 weeks after treatment has started to see if measurable changes have occurred in the tumor size. As a tumor is treated with effective therapies and the cell density of the tumor starts to dissipate, the random movement or the diffusion of water in the body tissue being treated increases.
In the Michigan study, those patients who had a high functional diffusion map score had a median survival of 52-53 weeks, while those with a low score had a median survival of 10 months.
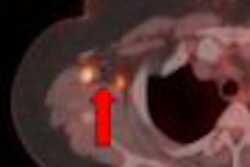
Ross called the trial results "promising," and urged the evaluation of functional diffusion mapping in a large multicenter clinical trial. He noted that the technology can be extended to tumors and cancers outside the brain, and his research group is already working on studies of functional diffusion mapping in lymphoma, sarcoma, head and neck cancer, and primary breast cancer, as well as prostate cancer that has metastasized to the bones.
According to Ross, functional diffusion mapping has several advantages: it's a quantifiable imaging parameter, it's available quite rapidly on any MRI machine, and its use shows consistent results across various MRI equipment manufacturers. In a 10-patient study performed over three weeks, Ross and his fellow researchers found the variability of functional diffusion mapping to be less than 2%.
In comments after Ross' presentation, Dr. Robert Gillies, Ph.D., of the Arizona Cancer Center in Tucson, noted that the statistics in the University of Michigan study were strong and the technology has the advantage of being noninvasive, since it uses endogenous contrast. He questioned, however, whether functional diffusion mapping could be useful for predicting outcome in patients other than those with glioma.
"It's too early to tell if these results can be extended to other cancers. But this should be considered a challenge, rather than an obstacle," he said.
Still, Ross believes that functional diffusion mapping has great advantages for patients suffering from a terminal illness -- for whom every day and week counts.
"If I were a patient undergoing treatment, I'd want to know the outcome of treatment as soon as possible, and functional diffusion mapping is potentially one way to provide that information, and plan more effective therapies," he said.
By Barbara Boughton
AuntMinnie.com contributing writer
April 22, 2008
Related Reading
MR perfusion imaging predicts malignant transformation of gliomas, March 27, 2008
Study shows benefits of very delayed cerebral FDG-PET imaging, December 21, 2007
Incidental findings on rain MRI common as technology advances, November 1, 2007
Genetic variation affects low-grade glioma response to temozolomide, May 24, 2007
Copyright © 2008 AuntMinnie.com