AuntMinnie.com is pleased to present the first installment of a three-part series on preventing infection in MRI by Dr. Peter A. Rothschild. The first part focuses on the growing problem of healthcare-associated infections and also details guidelines on infection control and MRI safety.
Healthcare- and community-associated infections are a growing problem in the U.S. and throughout the world. Healthcare-associated infections constitute a major U.S. public health problem: 5% to 10% of hospitalized patients are affected annually, resulting in about 2 million cases of healthcare-associated infections and 90,000 deaths, and adding $4.5 billion to $5.7 billion in healthcare costs.
Most patients with serious infections typically have some type of imaging procedure performed during the course of their treatment. Radiology departments and outpatient imaging centers must take appropriate action to assure patients that their MRI scanner is not a significant hub for microorganisms capable of causing infectious diseases.
However, for many reasons, MRI suites often lack the most basic safeguards against infection. Due to the unique environment, implementing and maintaining an effective infection control policy is extremely difficult. Because of the dangers from extremely strong magnetic fields -- as demonstrated by the well-publicized death of 6-year-old Michael Colombini from an accident in an MRI scanner -- housekeeping staff and most cleaning equipment are usually prohibited from entering the MRI suite. The resultant lack of thorough cleaning was clearly demonstrated in a 2006 study by researchers in Ireland who cultured methicillin-resistant Staphylococcus aureus (MRSA) from within the bore of an MRI system (Irish Journal of Medical Science, October 2005, Vol. 174:4, pp. es3:10).
When you go to a restaurant, you assume that it is clean -- that an organization (the county heath department) comes and inspects the restaurant to ensure food safety and cleanliness. However, for MRI, even though the public assumes the proper infection control procedures are in place, there is no one organization that evaluates MRI suites for infection control. I have often found, especially in freestanding outpatient centers and mobile MRI units, a complete lack of even basic infection control procedures, such as hand washing or cleaning the room between patients.
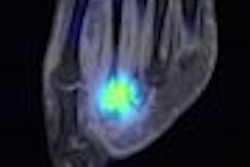
The pictures below illustrate just a few examples of how unbelievably dirty these MRI suites can be.
 |
| Cables in the MRI room. All images courtesy of Dr. Peter Rothschild. |
 |
| The floor of an MRI suite -- note that only the front half has been cleaned. |
 |
| An MRI-compatible aluminum IV pole. |
MRSA
Originally identified in 1961, MRSA is now widespread throughout healthcare facilities, in both hospital and outpatient settings. The most common source for MRSA transmission is by direct or indirect contact with people who have MRSA infections or are asymptomatic carriers.
In 1972, MRSA accounted for only 2% of all S. aureus infections, but now it is responsible for 50% to 70% of these infections. MRSA is among those microorganisms commonly referred to as a "super bug." MRSA may be community-associated (CA-MRSA) or healthcare-associated (HA-MRSA).
The morbidity and mortality of these bacteria are staggering. On average, hospitalization stays for treating MRSA versus other infections are approximately three times longer and three times more expensive. Additionally, the risk of death is three to five times greater for patients infected with MRSA versus methicillin-sensitive S. aureus.
A major concern for imaging centers is that MRSA can be carried by asymptomatic persons. Worldwide, up to 53 million people are estimated to be asymptomatic MRSA carriers; of these, an estimated 2.5 million reside in the U.S. Approximately 1% of the U.S. population is colonized with MRSA. Both infected and colonized patients contaminate their environment with the same relative frequency. Therefore, any patient lying on an imaging table could be a carrier capable of contaminating surfaces in the radiology suite. MRSA and other pathogens can live on inanimate surfaces such as common table pads and positioners for as long as several months.
Centers for Disease Control and Prevention (CDC)
The CDC has developed guidelines for environmental infection control in healthcare facilities. The CDC and the Healthcare Infection Control Practices Advisory Committee issued a 249-page document extensively detailing their recommendations concerning, in part, the principles of cleaning and disinfecting various surfaces, including those frequently found in radiology suites, such as bed linens, pillows, mattresses, carpeting, and cloth furnishings. The CDC cited numerous well-controlled studies indicating that MRSA can be spread by contaminated surfaces.
In a section regarding laundry and bedding, the CDC states: "Standard mattresses and pillows can become contaminated with body substances during patient care if the integrity of the covers of the items is compromised.... A linen sheet placed over the mattress is not considered a mattress cover. Patches for tears or holes in mattress covers do not provide an impermeable surface over the mattress.... Wet mattresses, in particular, can be a substantial environmental source of microorganisms. Infections and colonization by ... MRSA ... have been described...."
In a section titled "Epidemiology and General Aspects of Infection Control," the CDC provides detailed information about contaminated textiles and fabrics:
Contaminated textiles and fabrics often contain high numbers of microorganisms from body substances, including blood, skin, stool, urine, vomitus, and other body tissues and fluids. When textiles are heavily contaminated with potentially infective body substances, they can contain bacterial loads of 106-108 CFU/100 cm2 of fabric. Disease transmission attributed to healthcare laundry has involved contaminated fabrics that were handled inappropriately (i.e., the shaking of soiled linen). Bacteria (Salmonella spp., Bacillus cereus), viruses (hepatitis B virus [HBV]), fungi (Microsporum canis), and ectoparasites (scabies) presumably have been transmitted from contaminated textiles and fabrics to workers via a) direct contact or b) aerosols of contaminated lint generated from sorting and handling contaminated textiles.
American College of Radiology (ACR) safe MRI practices
The ACR has developed a document for safe MR practices, most recently revised in 2007. The ACR has divided the MRI area into four zones. The most critical is Zone IV, which is the magnet room itself. To enter this zone without supervision, the person should have level 2 MRI safety training.
The ACR defines level 2 MR personnel as "Those who have been extensively trained and educated in broad aspects of MRI safety issues including, for example, issues related to potential for thermal loading or burns and direct neuromuscular excitation from rapidly changing gradients." This is in addition to "successfully completing at least one of the MRI safety lectures or prerecorded presentations approved by the [site's] MR medical director." The ACR then states that this "should be repeated at least annually and appropriate documentation should be provided to confirm these ongoing educational efforts."
The ACR goes on to say that the MR medical director is responsible for identifying the necessary training and the individuals who qualify as level 2 MR personnel.
The ACR also specifically requires that any non-MR personnel entering the scan room must "be accompanied by, or under the immediate supervision of and in visual or verbal contact with, a specifically identified level 2 MR person for the entirety of the duration" within the scan room. Additionally, non-MR personnel, such as cleaners, must also go through a thorough screening to ensure that they do not have a pacemaker, aneurysm clip, or any other dangerous ferromagnetic objects in or on their body. This is why cleaning crews are normally not allowed to enter the scan room.
The number of accidents in MRI suites appears to be a growing problem. Between mid-2005 and mid-2006, the U.S. Food and Drug Administration saw a 140% increase in reported MRI accidents. MRI safety has become such an important topic that the ACR issued its revised MRI safety guidance document in 2007. In February 2008, the Joint Commission released a Sentinel Event Alert, "Preventing accidents and injuries in the MRI suite." Each of these documents emphasizes the importance of designating the various areas within the MRI area into Zones I through IV, depending upon the static magnetic field of each zone and the consequent safety precautions that must be taken in each one.
The most dangerous zones are the MRI control room, Zone III, and the MRI suite itself, Zone IV. Both Zone III and Zone IV are within "the region in which free access by unscreened non-MR personnel or ferromagnetic objects or equipment can result in serious injury or death," according to the ACR. The zones are considered dangerous enough that they "should be physically restricted from general public access by, for example, key locks, passkey locking systems, or any other reliable, physically restricting method that can differentiate between MR personnel and non-MR personnel.... Only MR personnel shall be provided free access, such as access keys or passkeys, to Zone III."
The major risks involve metallic objects being brought in by unauthorized and untrained personnel. The technologist who runs the MRI unit is responsible for this access control. Therefore, when the technologist is absent, all access should be denied to the MRI suite. This would include after-hours cleaning crews. The ACR guidelines discuss restrictions on housekeeping and cleaning personnel from Zones III and IV.
However, the 17 text pages of the ACR document contain only one paragraph on infection control:
Because of safety concerns regarding incidental personnel within the MR suite, restricting housekeeping and cleaning personnel from Zone III and/or Zone IV regions may give rise to concerns about the cleanliness of the MR suite. Magnet room finishes and construction details should be designed to facilitate cleaning by appropriately trained staff with nonmotorized equipment. Additionally, as the numbers of MR-guided procedures and interventional applications grow, basic infection control protocols, such as seamless floorings, scrubbable surfaces, and hand-washing stations, should be considered.
This paragraph confirms the widespread practice of restricting cleaning crews from entering the MRI suite. But I don't know of any imaging center or hospital that pays their level 2 MR personnel (i.e., the technologists) to wait around for the cleaning crews to come in and monitor them the entire time that they are cleaning the room. Therefore, the responsibility to clean the scan room is sometimes assigned to a MRI technologist or, more commonly, this responsibility is simply overlooked. However, the paradox is that the MRI technologist, who in almost all imaging centers is the level 2-trained person, is rarely an experienced or even trained cleaning person with very limited time to clean.
This paradox is clear when asking the question "Is the scan room being cleaned, and if so, by whom?" The answer that I normally receive is "Of course it's being cleaned by the cleaning crews that come in at night after we leave." It is crucial to ask the next question: "What level 2 personnel are present to monitor the cleaning crew to make sure that it is done properly and safely?" I don't know of any cleaning crew that has the background training to be level 2 personnel. Additionally, the cleaning crews I've contacted have all stated that they have been told or simply assume that they are not to go into the scan room. Cleaners often describe the MRI suite as the room with all the signs on the door warning them not to enter.
By Dr. Peter A. Rothschild
AuntMinnie.com contributing writer
June 20, 2008
Part II of the series will focus on steps to prevent infections in the MRI suite.
Dr. Rothschild is co-founder and medical director of High Field & Open MRI of Louisville, KY. He also is the president and founder of Patient Comfort Systems and Image Enhancement Systems, both in Hayward, CA. Since 1988, Rothschild has practiced exclusively in the area of MRI. He helped develop the first commercially available open MRI scanner while at the University of California, San Francisco, and pioneered the clinical aspects of open MRI, edited the first medical textbook on the subject, and has authored numerous medical journal articles about various aspects of MRI.
Related Reading
Sink or swim: Why a hand sink is crucial in the MR suite, March 14, 2008
Joint Commission MR safety surveys: Moving past the fire extinguisher, August 29, 2007
MR guidelines: Elevating standards of practice and care, May 10, 2007
MR suite level designations: Don't let complex procedures overwhelm your facility, March 27, 2007
How to calculate your MRI suite safety score, February 8, 2007
References
Blythe D, Keenlyside D, Dawson SJ, Galloway A. Environmental contamination due to methicillin-resistant Staphylococcus aureus (MRSA). J Hosp Infect. 1998;38(1):67-69.
Boyce JM, Potter-Bynoe G, Chenevert C, King T. Environmental contamination due to methicillin-resistant Staphylococcus aureus: Possible infection control implications. Infect Control Hosp Epidemiol. 1997;18(9):622-627.
Chaljub G, Kramer LA, Johnson RF III, Johnson RF Jr., Singh H, Crow WN. Projectile cylinder accidents resulting from the presence of ferromagnetic nitrous oxide or oxygen tanks in the MR suite. AJR. 2001;177(1):27-30.
Cosgrove SE, Qi Y, Kaye KS, Harbarth S, Karchmer AW, Carmeli Y. The impact of methicillin resistance in Staphylococcus aureus bacteremia on patient outcomes: Mortality, length of stay, and hospital charges. Infect Control Hosp Epidemiol. 2005;26(2):166-174.
Dietze B, Rath A, Wendt C, Martiny H. Survival of MRSA on sterile goods packaging. J Hosp Infect. 2001;49(4):255-261.
ECRI Institute. Patient death illustrates importance of adhering to safety precautions in magnetic resonance environments. Health Devices. 2001;30(8):311-314.
Engemann JJ, Carmeli Y, Cosgrove SE. Adverse clinical and economic outcomes attributable to methicillin resistance among patients with Staphylococcus aureus surgical site infection. Clin Infect Dis. 2003;36(5):592-598.
Gilk T, Bell R. The state of MRI safety. Imaging Economics Web site. http://www.imagingeconomics.com/issues/articles/2007-09_04.asp. September 2007. Accessed March 9, 2008.
Guidelines for Environmental Infection Control in Health-Care Facilities: Recommendations of CDC and Healthcare Infection Control Practices Advisory Committee (HICPAC). Centers for Disease Control and Prevention Web site. http://www.cdc.gov/ncidod/dhqp/gl_environinfection.html. June 2003.
Hardy KJ, Oppenheim BA, Gossain S, Gao F, Hawkey PM. A study of the relationship between environmental contamination with methicillin-resistant Staphylococcus aureus (MRSA) and patients' acquisition of MRSA. Infect Control Hosp Epidemiol. 2006;27(2):127-132.
Healthcare-associated infections (HAIs). Centers for Disease Control and Prevention Web site. http://www.cdc.gov/ncidod/dhqp/healthDis.html. Updated February 23, 2006.
Kanal E, Barkovich AJ, Bell C, et al. ACR Guidance Document for Safe MR Practices: 2007. AJR. 2007;188(6):1447-1474.
Karchmer TB. Editorial commentary: Prevention of healthcare-associated methicillin-resistant Staphylococcus aureus (MRSA) infections: Adapting to a changing epidemiology. Clin Infect Dis. 2005;41(2):167-169.
Kaye KS, Engemann JJ, Mozaffari E, Carmeli Y. Reference group choice and antibiotic resistance outcomes. Emerg Infec Dis. 2004;10(6):1125-1128. Available at http://www.cdc.gov/ncidod/eid/vol10no6/02-0665.htm.
Lodise TP, Rhoney DH, Tam VH, et al. Clinical and economic impact of methicillin resistance in patients with Staphylococcus aureus bacteremia. Diag Micro Inf Dis. 2005;52(2):113-122.
Lucet JC, Grenet K, Armand-Lefevre L, et al. High prevalence of carriage of methicillin-resistant Staphylococcus aureus at hospital admission in elderly patients: Implications for infection control strategies. Infect Control Hosp Epidemiol. 2005;26(2):121-126.
Peck P. Fatal MRI accident is first of its kind. WebMD.com. http://www.webmd.com/news/20010801/fatal-mri-accident-is-first-of-its-kind. August 1, 2001.
Preventing accidents and injuries in the MRI suite. Joint Commission Web site. http://www.jointcommission.org/SentinelEvents/SentinelEventAlert/sea_38.htm. February 14, 2008.
Salgado CD, Farr BM. What proportion of hospital patients colonized with methicillin-resistant Staphylococcus aureus are identified by clinical microbiology cultures? Infect Control Hosp Epidemiol. 2006;27(2):116-21.
Scanlon T, Murray J. MRSA detection in the radiology department. Ir J Med Sci. 2005;174(4),es3:10.
Soule BM. Avoiding the drama of hospital acquired infections. Hospitals & Health Networks Magazine Web site. http://www.hhnmag.com/hhnmag_app/jsp/articledisplay.jsp?dcrpath=HHNMAG/Article/data/01JAN2008/080129HHN_Online_Soule&domain=HHNMAG. January 29, 2008.
Understanding MRSA (methicillin resistant Staphylococcus aureus). WebMD.com. http://www.webmd.com/skin-problems-and-treatments/understanding-mrsa-methicillin-resistant-staphylococcus-aureus. Reviewed July 2, 2007. Accessed March 9, 2008.
Wagenvoort JH, Sluijsmans W, Penders RJ. Better environmental survival of outbreak vs. sporadic MRSA isolates. J Hosp Infect. 2000;45(3):231-234.
Whitby M, McLaws ML, Berry G. Risk of death from methicillin-resistant Staphylococcus aureus bacteraemia: A meta-analysis. Med J Aust. 2001;175(5):264-267.
Copyright © 2008 Dr. Peter Rothschild