Breast MRI is gaining increased clinical interest as both a screening and diagnostic tool: some studies show an average of 2.2% added cancer yield when MRI is performed in addition to mammography, and others have found that MRI detects contralateral, occult cancers in 3% of women with a recent breast cancer diagnosis.
But how many doctors are actually using the modality, and how are they using it? Researchers at the University of California, Los Angeles; the Washington University School of Medicine in St. Louis; and the University of California, San Francisco investigated the current practices of radiologists regarding the performance and interpretation of breast MRI in the hope that the data gathered could help develop practice guidelines and standardize the use and technical performance of the technology. Their findings will be published in an upcoming issue of the American Journal of Roentgenology (August 2008, Vol. 191:2, pp. 332-339).
Between September 2006 and January 2007, Dr. Lawrence Bassett and colleagues invited the 1,696 active physician members of the Society of Breast Imaging (SBI) to complete a survey that addressed whether and how they performed and interpreted breast MRI. The team garnered a total of 754 completed surveys (632 completed online, 122 received by mail).
Who uses breast MRI, and how available is it?
The study included 334 hospital-based outpatient facilities, 322 private outpatient facilities, 300 solely hospital-based facilities, 144 academic facilities, 25 county facilities, and seven military or veterans' facilities (many of the respondents' practices included more than one type of facility).
The majority of the practices that responded to the survey had high numbers of radiologists. There were:
- More than 20 radiologists in 292 practices
- 16 to 20 radiologists in 100 practices
- 11 to 15 radiologists in 90 practices
- 6 to 10 radiologists in 114 practices
- 4 to 5 radiologists in 32 practices
- 1 to 3 radiologists in 90 practices
Of these groups, the number of radiologists reading mammograms was one to three in 162 practices, four to five in 160, six to 10 in 238, 11 to 15 in 86, 16 to 20 in 39, and more than 20 in 34.
The technology was offered at 75.5% (569 of 754) of the practices that responded to this question.
What kind of techniques and protocols are out there?
Bassett and colleagues found that of the 553 facilities that responded to the question of breast MRI techniques and protocols, the majority (207 or 37.4%) performed fewer than five per week. Of the remaining practices:
- 167 (30.2%) did 5 to 10
- 79 (14.3%) did 11 to 15
- 44 (8%) did 16 to 20
- 22 (4%) did 21 to 25
- 10 (1.8%) did 26 to 30
- 8 (1.4%) did 31 to 35
- 11 (2%) did 35 to 50
- 5 (0.9%) did more than 50
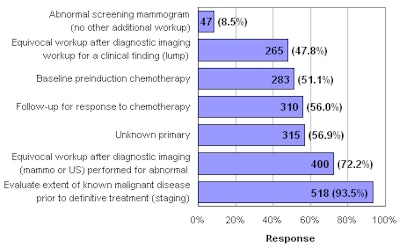
In response to the question, "What are the usual indications for a diagnostic breast MRI done in your practice?" the study found:
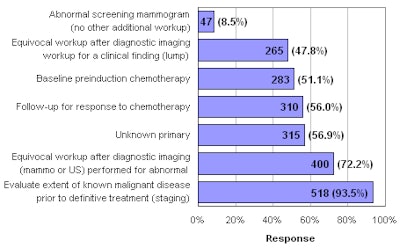 |
| Total percentage exceeds 100 because many respondents specified more than one indication for performing breast MRI. Bassett LW, Dhaliwal SG, Eradat J, et al. National trends and practices in breast MRI. AJR. 2008;191:332-339. All data courtesy of the American Roentgen Ray Society. |
In response to the question, "What are the indications for a screening breast MRI done in your practice?" the study found:
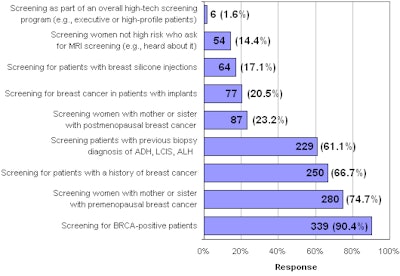 |
| ADH = atypical ductal hyperplasia, LCIS = lobular carcinoma in situ, and ALH = atypical lobular hyperplasia. Total percentage exceeds 100 because many respondents specified more than one indication for performing screening breast MRI. Bassett LW, Dhaliwal SG, Eradat J, et al. National trends and practices in breast MRI. AJR. 2008;191:332-339. |
The survey revealed that the technical aspects of performing breast cancer were not standardized; the majority of respondents (96.9%) indicated that they used 1.5-tesla magnets, but 9.5% used 3-tesla magnets, 2.9% used equipment designed for breast MRI, and 1.3% used magnets under 1 tesla.
As to how breast MRI exams were interpreted, 47.3% of the survey respondents stated a soft-copy workstation without computer-aided detection (CAD) was used, 7.4% said that soft-copy workstation with CAD was always used, 7.4% stated that a soft-copy workstation with CAD was sometimes used, and 2% said that hard copy was used. Of the practices that participated in the survey, 84% indicated that they never or rarely interpreted breast MRI without comparing its results with mammography and sonography exams.
Finally, the study found that academic practices were more likely than nonacademic practices to offer breast MRI (88.9% versus 70.3%) and perform screening breast MRI (83.2% versus 58.5%) and MRI-guided interventional breast procedures (83.3% versus 65.5%).
The researchers believe the survey data will help radiologists develop standardized breast MRI protocols.
"Hopefully, our study will help radiologists understand what other people are doing with breast MRI, and determine whether they're on track with the trend or on a totally different course," Bassett and colleagues wrote.
By Kate Madden Yee
AuntMinnie.com staff writer
July 24, 2008
Related Reading
Breast MRI helps rule out multifocal disease, plan treatment, July 18, 2008
Solid-state scintimammography matches breast MRI, July 2, 2008
High-spatial resolution SER imaging may improve breast cancer outcomes, July 2, 2008
When MRI won't work, MDCT can help differentiate breast lesions, study suggests, June 19, 2008
Contrast MRI helps track breast cancer therapy response, June 6, 2008
Copyright © 2008 AuntMinnie.com