Triple-negative (TN) breast cancer, in which the tumor is estrogen receptor negative, progesterone receptor negative, and human epidermal growth factor receptor 2 (HER2) negative, tends to be harder to diagnose, giving these women fewer treatment options and worse prognoses than those with non-TN tumors. Because of this, researchers are investigating whether TN breast cancer has any clinical markers that can be used to recognize it.
Dr. Takayoshi Uematsu, Ph.D., and colleagues at Shizuoka Cancer Center Hospital in Nagaizumi, Japan, conducted a study to determine specifically if certain MR characteristics can help radiologists identify triple-negative breast cancer. Their findings are published in this month's issue of Radiology (March 2009, Vol. 250:3, pp. 638-647).
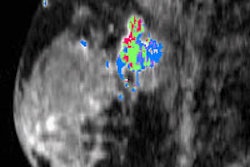
"Triple-negative breast cancer can mimic benign breast lesions, making it difficult for mammography or ultrasound to distinguish it," Uematsu told AuntMinnie.com via e-mail. "But breast MRI can reveal the cancer's intratumoral characteristics, such as necrosis and fibrosis."
The study included 176 women with surgically confirmed TN breast cancer; the mean age of the group was 56 years. MR exams were performed with a 1.5-tesla MR unit (Gyroscan Intera, Philips Healthcare, Andover, MA) with breast surface coils. Two radiologists with eight and 12 years of breast MR imaging experience read the images without knowing the surgical findings. Triple-negative breast cancer characteristics were compared to those of breast cancers that were estrogen receptor positive, progesterone receptor positive, and HER2 negative.
Women with triple-negative breast cancer were more likely to have histologically high-grade tumors and unifocal lesions than those who did not have it (86% versus 13.7% and 66% versus 46.2%, respectively).
| Characteristics of patients with triple-negative breast cancer and those with ER-positive/PR-positive/HER2-negative breast cancer | |||||
 |
|||||
| Characteristic | Triple-negative cancer (n = 59) | ER-positive/ PR-positive/ HER2-negative cancer (n = 117) |
P value | ||
 |
|||||
| Age (y)* | 60 (30-87) | 56 (29-83) | 0.253 | ||
 |
|||||
| Tumor size (mm)* | 21 (7-55) | 19 (10-70) | 0.139 | ||
 |
|||||
| Histologic tumor grade | < 0.001 | ||||
 |
|||||
| Low | 0 (0) | 23 (19.7) | |||
 |
|||||
| Moderate | 8 (14) | 78 (66.7) | |||
 |
|||||
| High | 51 (86) | 16 (13.7) | |||
 |
|||||
| Histologic tumor type | |||||
 |
|||||
| Invasive ductal carcinoma | 44 (75) | 98 (83.8) | 0.145 | ||
 |
|||||
| Invasive lobular carcinoma | 4 (7) | 11 (9.4) | 0.776 | ||
 |
|||||
| Medullary carcinoma | 7 (12) | 1 (0.9) | 0.002 | ||
 |
|||||
| Metaplastic carcinoma | 4 (7) | 0 (0) | 0.012 | ||
 |
|||||
| Mucinous carcinoma | 0 (0) | 7 (6.0) | 0.097 | ||
 |
|||||
| Axillary lymph node positivity | 21 (36) | 45 (38.5) | 0.711 | ||
 |
|||||
| Unifocal lesion | 39 (66) | 54 (46.2) | 0.012 | ||
 |
|||||
| Note: Unless otherwise indicated, data are numbers of patients, with percentages in parentheses. Percentages may not add up to 100% because of rounding. *Data are means, with ranges in parentheses. All data courtesy of the Radiological Society of North America. | |||||
As for lesion type, 95% of triple-negative breast cancer lesions showed as masses on MR, compared with 66.7% of non-TN cancers. Furthermore, the researchers found that triple-negative breast cancer lesions tended to show smooth mass margin, rim enhancement, persistent enhancement pattern, and very high intratumoral signal intensity on T2-weighted MR images.
| Comparison of MR imaging findings in mass lesion types between patients with triple-negative breast cancer and patients with ER-positive/PR-positive/HER2-negative breast cancer | |||||
 |
|||||
| MRI imaging finding | Triple-negative cancer (n = 56) | ER-positive/ PR-positive/ HER2-negative cancer (n = 78) |
P value | ||
 |
|||||
| Mass shape | 0.065 | ||||
 |
|||||
| Round | 10 (18) | 11 (14) | |||
 |
|||||
| Oval | 13 (23) | 30 (38) | |||
 |
|||||
| Lobulated | 23 (41) | 12 (15) | |||
 |
|||||
| Irregular | 10 (18) | 25 (32) | |||
 |
|||||
| Mass margin | 0.001 | ||||
 |
|||||
| Smooth | 22 (39) | 11 (14) | |||
 |
|||||
| Irregular | 34 (61) | 67 (86) | |||
 |
|||||
| Internal enhancement | < 0.001 | ||||
 |
|||||
| Homogeneous | 0 (0) | 2 (3) | |||
 |
|||||
| Heterogeneous | 11 (20) | 76 (97) | |||
 |
|||||
| Rim enhancement | 45 (80) | 0 (0) | |||
 |
|||||
| Intratumoral signal intensity on T2-weighted images | 0.002 | ||||
 |
|||||
| Low or equal | 30 (54) | 66 (85) | |||
 |
|||||
| High | 7 (12) | 3 (4) | |||
 |
|||||
| Very high | 19 (34) | 9 (12)* | |||
 |
|||||
| Pattern at dynamic enhancement imaging | 0.005 | ||||
 |
|||||
| Persistent | 24 (43) | 16 (21) | |||
 |
|||||
| Plateau | 4 (7) | 37 (47) | |||
 |
|||||
| Washout | 28 (50) | 25 (32) | |||
 |
|||||
| Note: Numbers in parentheses are percentages. Percentages may not add up to 100% because of rounding. *Of these nine lesions, seven were mucinous carcinomas. All data courtesy of the Radiological Society of North America. | |||||
One of the surprising findings in the study was the time-signal intensity curve pattern of triple-negative breast cancer, Uematsu told AuntMinnie.com.
"Initially, rapid enhancement and a washout pattern is generally regarded to be a malignant pattern on breast MR imaging," he wrote in an e-mail. "However, this doesn't apply to triple-negative breast cancers. This different enhancement pattern may come from the heterogeneity of the triple-negative breast cancer."
Another surprising finding? Dynamic contrast-enhanced breast MR imaging with T2-weighted images works to identify this type of cancer, according to Uematsu. Of course, tissue samples are still important.
"This technique can increase the specificity of breast MR imaging because of correlation of intratumoral necrosis with the hyperintense area on T2-weighted images," he wrote. "But breast MR imaging with imperfect positive predictive values and negative predictive values cannot replace tissue samples."
By Kate Madden Yee
AuntMinnie.com staff writer
March 10, 2009
Related Reading
Triple-negative breast cancers show marked clinical features, November 29, 2007
Triple-negative breast cancers more likely to affect young, poor minority women, April 13, 2007
Prognostic markers in triple-negative breast cancer identified, February 15, 2007
Protein could help detect aggressive breast cancer, January 26, 2007
Copyright © 2009 AuntMinnie.com