MRI is an efficient diagnostic tool to evaluate testicular masses and accurately differentiate between benign and malignant intratesticular tumors, according to a study published in the March issue of the American Journal of Roentgenology.
The research from University Hospital of Ioannina in Greece also found that MRI can estimate the local extent of disease in patients with malignant tumors. The lead author of the study, Dr. Athina Tsili, is from the hospital's department of clinical radiology (AJR, Vol. 194:3, pp. 682-689).
Although sonography traditionally has been the primary imaging modality to evaluate scrotal contents, the authors noted previous research indicating the technology does not always offer "confident characterization" of the nature of testicular masses.
MRI, on the other hand, can simultaneously image both testicles and both sides of the inguinal region and provides adequate anatomic information and tissue contrast. Past studies also have concluded that MRI may be beneficial when sonography's results are equivocal or inconclusive for testicular disease.
Patient enrollment
For the current study, the researchers enrolled 33 patients with a mean age of 35 years, ranging from 17 to 70 years. All patients had the presence of masses conformed by surgery, pathology, or both. Radical orchiectomy was performed on 29 patients, three patients had a testicular biopsy, and one patient had both radical orchiectomy and biopsy of the contralateral testis.
MRI scans were performed on a 1.5-tesla system (Gyroscan and Intera, Philips Healthcare, Andover, MA), with a 17-cm circular surface coil used with 27 patients and a pelvic phased-array coil with the other six patients. The patients were examined in the supine position, and gadolinium contrast was administered intravenously in all cases.
Two radiologists blinded to the surgical and histopathologic results interpreted the MR images. The researchers also recorded the presence or absence of intratesticular lesions and evaluated tumor size, signal homogeneity or heterogeneity, and patterns of contrast enhancement, among other variables.
Lesion detection
Through surgery and histopathologic examination, the study tallied 36 intratesticular lesions among the 33 patients. Of those 36 masses, 28 (78%) lesions were malignant, while eight lesions (22%) were found to be benign.
Within the group, 27 patients had intratesticular malignant tumors, three patients had benign testicular lesions, two patients had benign intratesticular masses in both testicles, and one patient had both a malignant and a benign testicular lesion.
| MRI for diagnosing malignant testicular tumors
|
The mean diameter of testicular neoplasms detected at MRI was 5.2 cm, ranging from 1.1 to 12 cm, "which was in accordance with the histopathologic results," the authors noted.
In addition, MRI showed its prowess in accurately staging the tumors. Twelve (92%) of 13 category T1 testicular tumors were correctly staged by MRI, while the modality accurately assessed the local extent of 11 (92%) of 12 category T2 malignant testicular tumors.
The authors noted one major limitation of the study: "Although all patients underwent both sonography and MRI evaluation of the scrotum, no direct evaluation of the results with these techniques was performed," they stated. "A comparison of the diagnostic performances of sonography and MRI might justify the role of MRI compared with ultrasound in the diagnosis and characterization of testicular disease."
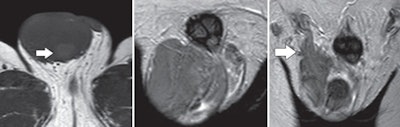 |
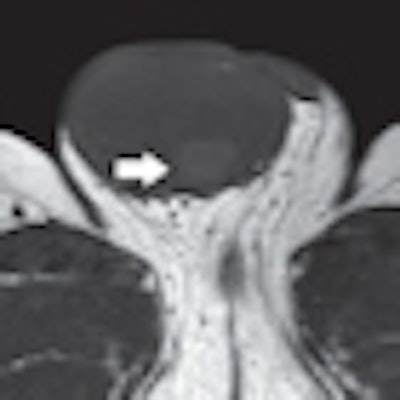
| Images are of a 40-year-old man with right testicular seminoma invading the spermatic cord. Left: Transverse T1-weighted MR image of a large right testicular tumor. The area of high signal intensity (arrow) within the lesion corresponds to histopathologic finding of hemorrhage. Center and right images are coronal T2-weighted MR, depicting a tumor of mainly low signal intensity invading the distal part of the ipsilateral spermatic cord (arrow). All images courtesy of the American Journal of Roentgenology. |
Based on the results, the researchers concluded that MRI is an "efficient diagnostic tool for the evaluation of testicular masses," adding that the modality is "accurate in the preoperative differentiation of benign and malignant intratesticular masses, facilitating accurate estimation of the local extent of disease in patients with malignant tumors."
By Wayne Forrest
AuntMinnie.com staff writer
March 4, 2010
Related Reading
Chemotherapy effective for testicular seminoma, November 11, 2008
Single-dose carboplatin as effective as radiation for early testicular cancer, June 4, 2008
Testicular cancer therapy affects risk of second malignancies and CVD, October 26, 2007
Testicular cancer survivors face long-term increased risk of second cancer, September 21, 2005
Testicular cancer on the rise in much of the world, June 29, 2005
Copyright © 2010 AuntMinnie.com




















