MRI can reliably detect, precisely localize, and accurately characterize scrotal lesions to advance treatment strategies and avoid unnecessary surgery for patients, enabling many to save their testicles, according to a study in the September issue of the American Journal of Roentgenology.
In a retrospective survey of 84 patients, MRI achieved sensitivity, specificity, and positive and negative predictive values of 100% for the localization of scrotal lesions and in the analysis of testicular lesions' patterns. Lead study author is Dr. Oliver Mohrs from the department of cardiovascular imaging at Alice Hospital and Darmstadt Radiology in Darmstadt, Germany (AJR, Vol. 199:3, pp. 609-615).
Rising incidence
Mohrs and colleagues noted in their study that cases of testicular cancer have been on the rise, almost doubling in the past 40 years. The standard diagnostic pathway for assessing urologic symptoms involves manual palpation and sonography. However, while intratesticular masses are often malignant, findings can be contradictory or inconclusive due to sonography's limited capability, the authors wrote.
But with the correct diagnosis and characterization of scrotal and testicular masses, patients can be directed to the most appropriate treatment and avoid removal of the testicles, a procedure known as orchiectomy. While MRI could be a good tool to better characterize scrotal disorders, previous research on the topic is limited, the authors noted.
The researchers decided to investigate the topic in a study that involved 63 patients who underwent MRI with a 1.5-tesla system (Magnetom Avanto, Siemens Healthcare) and in 21 patients with a 1-tesla system (Signa, GE Healthcare).
The scrotal imaging protocol included axial fat-suppressed T1-weighted turbo spin echo (TSE), coronal T1-weighted spin echo, axial fat-suppressed T2-weighted TSE, and coronary fat-suppressed T2-weighted TSE. Patients received 0.1 mmol/kg of body weight of gadopentetate dimeglumine (Magnevist, Bayer HealthCare Pharmaceuticals) approximately one minute prior to axial and coronary fat-suppressed T1-weighted TSE images.
Two radiologists and one urologist were blinded to all clinical data and rated the MR images on a scale of 1 to 4, with 1 designated as poor and 4 rated as excellent. The reviewers evaluated a total of 165 scrotal compartments containing testicles in 84 patients.
Their cumulative analysis resulted in a mean overall image quality with MRI of 3.2 ± 0.7 points on the four-point scale. A total of 30 cases were rated as excellent, 42 results were considered good, 12 image sets were considered moderate, and one case was evaluated as poor.
MR image comparison
Mohrs and colleagues compared the MRI data with histopathologic results in 22 cases, which included the surgical report in one case, and with medical reports and scrotal ultrasound, follow-up, or laboratory results for 61 patients.
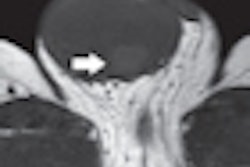
On the basis of the reference diagnosis, 70 patients had a clinically identified culprit lesion in a single compartment, and five patients in both compartments, resulting in a total of 80 scrotal lesions containing neoplasms in eight cases, traumatic lesions in six cases (one case of hemorrhage and five of scrotal hematoma or hematocele), inflammatory lesions in 36 cases (epididymitis, 22 cases; epididymo-orchitis and orchitis, six cases; aftermath of inflammation, two cases; and abscess, six cases), and tumor-like lesions in 25 cases.
With the help of MRI, researchers identified 80 clinically identified lesions in the 165 scrotal compartments, categorizing them as either testicular (28 lesions) or extratesticular (52 lesions), compared with the reference diagnosis. The findings achieved 100% sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV).
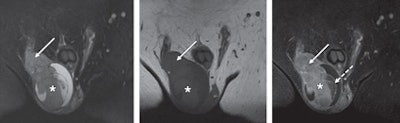 |
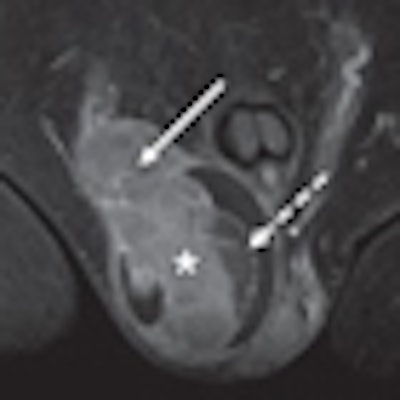
| A 66-year-old man with right-sided seminoma (asterisk), correctly localized and characterized with MRI. Coronal T2-weighted fat-suppressed (left), T1-weighted (center), and T1-weighted fat-suppressed contrast-enhanced (right) MR images show multinodular configuration with enhancing septa of mass and infiltration of tunica albuginea, epididymis, and spermatic cord (solid arrow). Noninfiltrated part of testicle has necrotic nonperfused parenchyma after contrast enhancement (dashed arrow). Images courtesy of AJR. |
The individual pattern of the 28 testicular lesions was correctly analyzed as cystic, solid, mixed, edema, hemorrhagic, or tunical involvement in all cases. Once again, sensitivity, specificity, NPV, and PPV were 100%.
Among the 52 extratesticular lesions, the solid pattern was described correctly by MRI in all 52 cases. A total of 12 lesions with a cystic pattern were correctly classified. However, there were two cases in which cystic lesions resulted in a false-positive result. Sensitivity was 87%, specificity rated 97%, PPV was 80%, and NPV was 97%.
MRI correctly identified all seven malignant lesions, but two cases were classified as false positives. Of the 73 benign lesions, 27 lesions (37%) were correctly identified as tumor-like lesions, with two false positives and one false-negative result. Inflammatory lesions were deemed true-positive among 44 cases, with false positives in three individuals and false negatives in four results.
Based on the results, Mohrs and colleagues concluded that MRI is "reliable in the detection of scrotal lesions and can differentiate scrotal disorders into testicular or nontesticular scrotal lesions."
"In this study, the differential diagnosis was narrowed on the basis of the MRI findings, and some lesions, such as dilated rete testis and seminoma, were identified directly," they wrote. "The study findings are of clinical importance, because more precise treatment strategies can be determined and orchiectomy avoided."