Results of a new study indicate that whole-body MRI is an excellent way to work up newly diagnosed breast cancer patients. Researchers from India found that MRI led to a change in treatment in nearly half of patients, and it also found metastases in some patients before symptoms appeared.
Faced with the need to evaluate breast cancer patients for metastases but lacking a PET/CT scanner at their center, radiologists at Deenanath Mangeshkar Hospital and Research Center in Pune, India, turned to whole-body MRI, ultimately learning that the modality offers a lot of value for the 70 minutes it takes to complete each scan.
"Ours was a fact-finding study to determine the utility of a comprehensive whole-body MRI protocol for metastasis workup in patients with breast cancer," said Dr. Joshita Singh in a presentation on Thursday at the 2010 American Roentgen Ray Society (ARRS) meeting. "The reason to choose patients with breast cancer is because we know that carcinoma of the breast is a systemic disease from the start."
Singh and her colleague Dr. Dhananjay Kelkar retrospectively analyzed MRI data in 99 patients examined between May 2005 and September 2009. Each patient underwent whole-body MRI at the initial workup and at follow-up, and 30 patients also had MRI for TNM (tumor, node, metastasis) staging, for a total of 114 studies in the 99 patients.
When a patient underwent MRI more than once, it was the first study that was used to classify the patient into either positive or negative for metastases, Singh said.
"For cancer care, we know that disease-free survival is our most important objective," she said. "Therefore, we used clinical follow-up as the primary end point for performance of MR as a metastasis workup tool. What it meant was that if the patient had MR done and we said the patient was nonmetastatic, and the patient continued to be disease-free at follow-up, it was used as a corroboration of the MR findings."
Therefore, the study required no comparisons with simultaneous alternate imaging modalities, or pathological confirmation of MRI findings. The median follow-up was 15.8 months, with a range of 0.5 to 57 months.
MR images were acquired using a 1.5-tela scanner enabled with total imaging matrix (Tim) and parallel acquisition. The average study time was 70 minutes, and patients also received a plain helical CT scan of the chest, a region for which CT has been shown to offer higher sensitivity than MRI for subcentimeter lung nodules, Singh said.
Of the total 99 patients, 47 were positive for metastasis and 52 were negative at the initial workup. Of these, a total of 46 patients remained disease-free at a median follow-up of 21.8 months, Singh said. Five developed metastases on follow-up MRI, and one patient was lost to follow-up.
Disease course in the five patients who developed metastases showed that the interval between the initial MRI and the development of metastases was fairly long.
Of the 47 patients who were positive for metastases, 35 died at a median time of four months postdiagnosis; two were still alive as of last month but have seen their disease progress despite treatment. Ten patients received appropriate treatment and have the disease under control at a median follow-up of 17.5 months, Singh said.
Bone, lung, liver, and brain were the primary metastasis sites among the 47 patients positive for metastasis at MRI.
MRI results in treatment changes
MRI detected metastases in 13 of 30 patients for the initial TNM staging, meaning that MRI upstaged the disease in 43% of patients, leading to a change in treatment. Whole-body MRI also detected metastases in nine of 38 follow-up studies in asymptomatic patients.
"It's debatable whether it's of any good use to detect metastases earlier than symptoms in the follow-up scenario, but the importance of this information lies in extrapolation to better metastasis workup in initial TNM staging," Singh said.
Whole-body MRI also detected additional metastatic sites in 11 symptomatic patients on follow-up and detected bone metastases earlier than symptoms in eight patients.
There were two false negatives in the 99-patient cohort, including one patient who had coexistent pulmonary tuberculosis. Whole-body MRI at the TNM staging missed a solitary subcentimeter lung nodule that was detected on asymptomatic follow-up whole-body MRI more than 30.5 months after the initial diagnosis -- a finding attributed to image interpretation error.
A second patient whose whole-body TNM staging exam was suggestive of lung metastasis developed leptomeningeal metastasis and came back to the center with seizures less than three months after diagnosis.
The single false-positive exam involved a patient with a solitary bone metastasis at the initial TNM staging seen as an enhancing lesion at MRI and staged as M0. This patient remains asymptomatic 23 months later, and follow-up MRI revealed the lesion to be unchanged, so it's probably benign, Singh said.
The study limitations included its retrospective design, lack of randomization, and selection bias at the clinician level, where patients were enrolled if they were considered likely to benefit from the protocol. There were no confirming studies with other modalities, and newer whole-body MRI advances such as diffusion-weighted imaging (DWI) were not incorporated, Singh said.
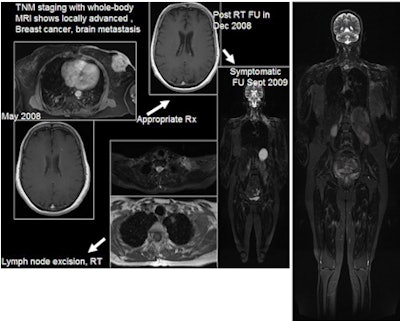 |
| 61-year-old woman with locally advanced breast cancer underwent whole-body MRI (far right), which revealed a brain metastasis. The patient initiated whole-brain radiation therapy and returned nine months later with neck pain, at which time repeat whole-body MRI showed lymphadenopathy and a solitary lung nodule. MRI is used to guide treatment of the patient, who now has her disease under control. Images courtesy of Dr. Joshita Singh. |
"Whole-body MRI with a dedicated individual organ imaging protocol has high accuracy for detection of brain, liver, and bone metastases," Singh said. "When supplemented with plain helical CT acquisition of chest, the protocol has high accuracy for lung metastases detection."
By Eric Barnes
AuntMinnie.com staff writer
May 11, 2010
Related Reading
Breast MRI improves cancer staging for newly diagnosed women, May 3, 2010
Whole-body MRI helps predict course of asymptomatic myeloma, March 18, 2010
California researchers create new breast PET/CT system, September 1, 2009
Whole-body MRI helps evaluate spondylarthritis, July 24, 2009
MRI sees spinal metastases earlier, but low-dose whole-body MDCT aces skeletal workup, May 20, 2005
Copyright © 2010 AuntMinnie.com




















