SAN FRANCISCO - Lung volumes in late gestation as measured by MRI are a key predictor of survival in infants with isolated congenital diaphragmatic hernia (CDH), according to research presented this week at the American Academy of Pediatrics (AAP) meeting.
Larger lung volumes when measured on MRI not only conferred a better chance of survival, they predicted whether infants might need extracorporeal membrane oxygenation (ECMO) support at birth, said investigators from Cincinnati Children's Hospital.
"At 34 weeks, parents will have this information, and they'll have an idea of how sick their kids are going to be," principal investigator Timothy Lee, MD, told AuntMinnie.com after the October 3 presentation.
CDH affects approximately one in 3,000 live births. In CDH the primary diagnostic indicator has been the lung-to-head (LHR) ratio at early gestation. However, recent literature suggests that there may be a role for fetal MRI lung volumes in predicting postnatal survival.
Previously, fetal MRI scans have been acquired as early as 25 weeks. "However, the majority of lung growth has not been completed until about 34 weeks' gestation, and our hypothesis was that prenatal imaging at this time might be a better assessment of the degree of pulmonary hypoplasia in this patient population," Lee said.
Lee, along with Foong Lim, MD, Sundeep Keswani, MD, and colleagues, from Cincinnati Children's Hospital and the University of Cincinnati, evaluated 67 CDH patients prenatally and treated them at the hospital. The study aimed to determine whether there was a correlation between late gestational fetal MRI-derived total lung volumes and CDH outcomes.
Fetuses with genetic or congenital cardiac abnormalities were excluded, leaving 44 patients. In addition:
- All patients were treated by an intradisciplinary CDH team.
- Ventilator management consisted of gentilation, high-frequency oscillatory ventilation, or biventilation.
- ECMO support was initiated by the CDH team attending and the ECMO surgeon.
- Hernias were repaired using either a Gore-Tex patch, transversus abdominal muscle flap, or primary repair.
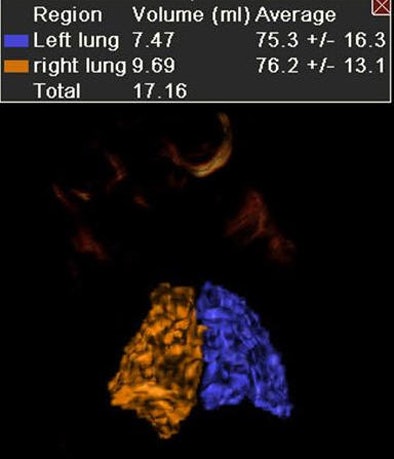
Multiplanar fetal MRI images were acquired on a 1.5-tesla MRI scanner (Signa, GE Healthcare, Chalfont St. Giles, U.K.). All images were reviewed by one of four fetal radiologists; a single technician calculated lung volumes by summation of the right and left lung volumes, minus the volume of the hernia and the mediastinal content, Lee said.
The average gestational age at birth was 37 6/7 weeks (range, 34-39 5/7). Of the 44 patients analyzed for the study, 39 were left-sided CDH and five were right-sided, and liver herniation was present in 26 patients (59%). The average total lung volume (TLV) was 27.7 mL ± 11.8, with an LHR ratio of 1.12 ± 0.32.
Lung volume and survival
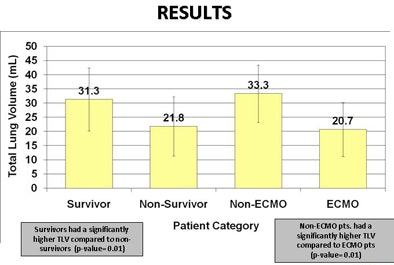
Total late-gestation lung volume for survivors was 31.3 mL ± 11 versus 21.8 mL ± 10.4 for nonsurvivors (p = 0.01), Lee said. Similarly, mean total lung volume for patients needing ECMO support was 20.7 mL ± 9.5 versus 33.3 mL for patients who did not need ECMO.
"With regard to survival, there was a significantly higher total lung volume for survivors compared to nonsurvivors, and the same was true of patients that did not need ECMO versus patients that needed ECMO," Lee said.
In all, 18 patients required ECMO, and the results showed a significant association between lower lung volumes (20.7 mL ± 9.5) and the need for ECMO (p = 0.0001).
Patients with total lung volume greater than 40 mL had a 90% chance of survival, while those with TLV less than 20 mL had a 35% chance of survival. As for ECMO, if total lung volume was less than 20 mL, then 86% of patients needed ECMO, compared to 25% for those with TLV 20-40 mL. Only 10% with TLV greater than 40 mL needed ECMO, Lee said.
 |
| Above, MRI of left lung (outlined in red) in CDH patient. Below, 3D reconstruction of normal lungs by fetal MRI. All images courtesy of Timothy Lee, MD. |
 |
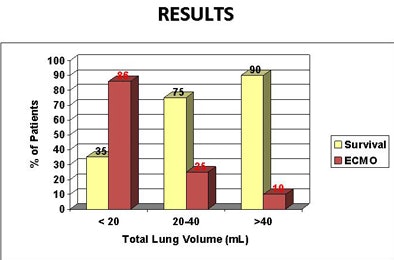 |
| Above, results showed significantly better survival and less use of ECMO in patients with higher lung volumes. Below, survivors and patients not needing ECMO had significantly higher mean total lung volumes. |
 |
Receiver operator characteristics (ROC) analysis for survival showed an area under the curve (AUC) of 0.736, with sensitivity and specificity of 64% and 85%, respectively. The same ROC analysis for patients on ECMO showed an AUC of 0.83, with sensitivity and specificity of 72% and 92%, respectively. Finally, TLV was inversely correlated with length of hospital stay.
Because fetal MRI measurements demonstrate significant correlations for survival, the need for ECMO support, and length of stay, "this test may be beneficial in counseling of expectant mothers who have children with isolated congenital hernias," Lee said.
The study's limitations included its retrospective design, and the outcomes may also be institution-specific, Lee said, meaning that the study should be replicated prospectively and in a multi-institutional setting.
An audience member said it would be difficult to translate the TLV results into advice for parents.
"What counseling do you do with this?" the audience member asked. "I imagine the [results] significantly overlap, and I would be hesitant to recommend for the ones with the biggest lung volumes that they not be born in an ECMO center because there's a 10% chance they could need it. But at the lower end, there are survivors, and I don't think you want to counsel them not to use ECMO."
Lee said it was certainly easier to make recommendations for the TLV results at either extreme than for those in the middle.
"But I think that patients coming in for prenatal counseling are very well educated -- they've looked at the literature, and what they want in regard to prenatal counseling is just an idea of where the child is going to be, what is going to be the course," Lee said. "If they're in the most severe group you can make the argument that there are centers around the country that do offer fetal interventions."
Tracheal balloons aren't yet used in the U.S., but there are other available tools, he said. Fetal lung volume "gives you at least an idea of where they will fall in the clinical realm postnatally, so if you have a child that's TLV less than 20, you're not going to flail that child with conventional measures -- you know that child is probably going to need to go to ECMO."
By Eric Barnes
AuntMinnie.com staff writer
October 7, 2010
Related Reading
MR amniotic fluid spectroscopy assesses late gestational age, May 28, 2010
320-row CT minimizes dose in pediatric abdominal studies, March 3, 2010
MRI outperforms ultrasound for fetuses with ventriculomegaly, November 10, 2009
3D ultrasound predicts fetal pulmonary hypoplasia, April 21, 2006
MRI shows promise for evaluation of neonatal respiratory problems, May 27, 2004
Copyright © 2010 AuntMinnie.com