Taiwanese researchers have found that measuring bone marrow perfusion with dynamic contrast-enhanced (DCE) MRI in acute myeloid leukemia patients in complete remission can help predict future outcome and survival, according to a study published online January 6 in Radiology.
With the information, DCE-MRI could be useful in determining at-risk acute myeloid leukemia patients and contribute to the development of more personalized treatment, the researchers from the National Taiwan University Hospital and College of Medicine reported. The lead study author is Bang-Bin Chen, MD, from the departments of medical imaging and radiology at the university.
The prospective study examined 112 patients with newly diagnosed acute myeloid leukemia from September 2004 to October 2007 at the Taiwan facility. Chemotherapy was the standard treatment for 96 patients, while the remaining 16 patients received more conservative treatment due to older age or other social or religious reasons.
The patient population included 49 women with a mean age of 45.4 years (range, 17 to 80 years) and 47 men with a mean age of 46.2 years (range, 16 to 75 years). The researchers then narrowed the study group to 51 patients who achieved complete remission and agreed to undergo the DCE-MRI scan.
DCE-MRI protocol
Spine MRI was performed using a 1.5-tesla MRI system (Magnetom Sonata, Siemens Healthcare, Erlangen, Germany) with a phased-array spine coil. Patients also received an injection of gadodiamide (Omniscan, GE Healthcare, Chalfont St. Giles, U.K.) at 0.15 mmol/kg based on body weight.
The time varied between complete remission and when the DCE-MRI was performed; however, the majority of patients -- 42 (82%) of the 51 -- received DCE-MRI scans within 100 days of achieving complete remission. The median follow-up time was 25.9 months after initial diagnosis.
To help evaluate outcome and survival, the researchers measured five MR pharmacokinetic parameters at each vertebral level. Two criteria were semiquantitative (peak and slope) and three were quantitative (amplitude, efflux rate constant [Kep], and elimination rate constant [Kel]). Each patient's overall survival and relapse-free survival rates also were assessed.
Survival calculations
Clinical parameters, including age, sex, time required to achieve complete remission, duration between complete remission and DCE-MRI scans, and DCE-MRI parameters at various vertebrae, were compared between acute myeloid leukemia patients who achieved complete remission without a relapse and those who had relapsed.
In their analysis, Chen and colleagues found that high values of peak (≥ 0.42), slope (≥ 0.0235), amplitude (≥ 0.03), and Kep (≥ 0.0082) were associated with shorter overall survival (p = 0.004, 0.01, 0.034, and 0.026, respectively). A high value of Kep also was associated with shorter relapse-free survival.
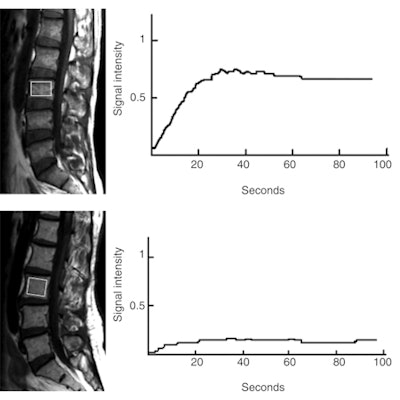 |
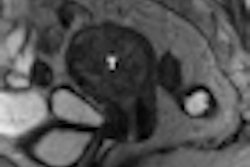
| Top image is of a 47-year-old man with early relapse after complete remission, with relapse-free survival of 179 days. High value for peak is 0.71 and Kep is 0.022. Bottom image is of a 62-year-old woman with low value for peak (0.15) and Kep (0.0024), who remained in remission until November 2009 and had relapse-free survival of 1,674 days. Images courtesy of Radiology. |
The cutoffs for high and low values for DCE-MRI pharmacokinetic parameters in patients at complete remission status were set as 0.42 for peak, 0.0235 for slope, 0.03 for amplitude, 0.0082 for Kep, and 0.0975 for Kel.
Chen and colleagues concluded that DCE-MRI of vertebral bone marrow in acute myeloid leukemia patients provides useful information on clinical outcome of patients who achieve complete remission. All DCE-MRI parameters were significantly associated with overall survival, as is high Kep, an indicator of overall survival and relapse-free survival.
"Patients with a higher value for Kep at complete remission would have shorter relapse-free duration and may need to undergo additional therapy," the authors added. "These parameters could serve as a guide for the selection of optimal management plans in acute myeloid leukemia patients, thereby contributing to the development of 'personalized medicine' for each patient."
The study cited several limitations, including the fact that no histologic data from bone marrow biopsy were available that could be correlated with MRI parameters in patients in complete remission. However, the authors noted that all patients underwent bone marrow aspiration at remission status, which showed no significant relationship of blast counts and cell differentiation with MRI parameters.
| Lead author Chen did not list any financial conflict-of-interest disclosures, nor did any of the study's co-authors. The study was supported by grants from the National Science Council and National Taiwan University Hospital. |
By Wayne Forrest
AuntMinnie.com staff writer
February 2, 2011
Related Reading
Childhood radiation exposure may increase risk of leukemia, October 6, 2010
PET-based F-18 FLT equivocal for leukemia imaging, January 7, 2009
Leukemia risk increases after breast cancer therapy in older women, September 25, 2007
Copyright © 2011 AuntMinnie.com