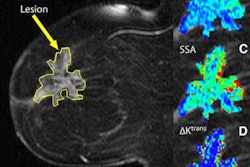
An MRI scan after initial chemotherapy and before surgery may predict long-term outcome for patients with advanced rectal cancer and identify individuals who could benefit from more aggressive therapy prior to surgery, according to a study published online August 29 in the Journal of Clinical Oncology.
Findings from the Magnetic Resonance Imaging and Rectal Cancer European Equivalence Study (MERCURY) study indicate that an MRI before surgery could help patients in several ways, such as by guiding more intense therapy or alternative chemotherapy for patients who initially appear resistant to chemotherapy treatment.
The research marks the first time that MRI has been shown to predict outcome for patients with rectal cancer who have completed initial chemoradiation therapy, according to lead study author Dr. Gina Brown, a consultant radiologist in the department of radiology at the Royal Marsden Hospital NHS Trust in Sutton, U.K.
MRI staging and reassessment of rectal cancers before and after chemoradiotherapy are not routinely done for all patients. However, the study has shown that using MRI for this application can help change the course of patient care, and may help some patients avoid surgery.
The MERCURY study measured tumor shrinkage in 111 patients who previously received preoperative radiotherapy or both chemotherapy and radiation for locally advanced rectal cancer. The patient population, which is part of a larger study of MRI use in improving rectal cancer staging begun in 2002, was then followed for the next five years.
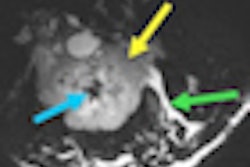
The researchers calculated the status of the cancer by tumor regression grade (TRG), which measures the degree of tumor decrease after therapy, and by circumferential resection margin (CRM), which shows the remaining cancer at the tumor edges after treatment or what is expected to remain after surgery. Patients were categorized as either "good" or "poor" responders to chemoradiation, based on the MRI.
Brown and colleagues found that 72% of good responders to chemotherapy/radiation were alive after five years, compared with 27% of patients among the poor responders to treatment. In addition, the disease-free survival for good responders was 64%, compared with 31% for the poor responders.
The researchers also found that local recurrence rate at five years for those patients for whom there was MRI-predicted CRM involvement was 28%, compared with 12% for patients with predicted cancer-free tumor margins.
Of the 111 patients in the study, 81 patients (73%) were expected to have cancer left in the surgical margins prior to initial treatment. After neoadjuvant therapy, only 47 patients (42%) were expected to have disease remaining in the surgery margins, which means this patient group remains at risk for recurrence prior to surgery.
Brown noted that future trials might be able to identify a subgroup of patients that has good response and for whom chemotherapy alone might be enough, while also identifying those who needed further therapy prior to surgery.



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)
.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)