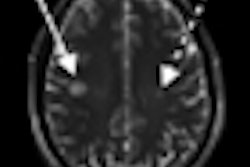
A new study published online February 20 in Archives of Neurology suggests that 7-tesla MRI with a specialized protocol is highly sensitive for detecting plaques in white and gray brain matter in patients with multiple sclerosis (MS).
German researchers used 7-tesla MRI with a T1-weighted magnetization-prepared rapid acquisition and multiple gradient-echo (MP-RAGE) technique. They found that the protocol "clearly delineated every cortical lesion" that was visualized by any other MRI sequence at 1.5 or 7 tesla. The lead author of the study was Tim Sinnecker, from the NeuroCure Clinical Research Center at Charité Medical University in Berlin.
T2-weighted MRI is often used to quantify accumulated MS lesions in the brain, while T1-weighted sequences are used to differentiate, among other things, irreversible brain tissue damage commonly called black holes, the authors wrote. Black holes are associated with the progression of MS and cerebral atrophy. On spin-echo T1-weighted images, a proportion of T2 hyperintense lesions (black holes) appears hypointense to the surrounding normal-appearing white matter for a long time, the group added.
The study included 20 patients with relapsing-remitting multiple sclerosis from the outpatient clinics of the NeuroCure Clinical Research Center. There were 11 male and nine female patients with a mean age of 42 years and mean disease duration of 3.1 years (range, 0.5 to 14.4 years).
For comparison purposes, 14 healthy control subjects also were enrolled. All 34 subjects underwent brain scans with a 7-tesla MRI system (Magnetom, Siemens Healthcare), using a 24-channel head coil. In addition, a subgroup of 18 patients with MS received brain scans with a 1.5-tesla system.
The imaging protocol included 2D T2-weighted fast low-angle shot (FLASH) and turbo inversion-recovery magnitude (TIRM) sequences. For 3D T1-weighted imaging, the researchers used the MP-RAGE sequence.
A reader blinded to the data independently evaluated each sequence. In a second study, all detected lesions were retrospectively analyzed in a side-by-side comparison of all sequences.
The analysis found that 7-tesla MP RAGE detected a total of 728 lesions, compared with 584 lesions with 7-tesla FLASH and 399 lesions with 1.5-tesla MP RAGE.
In addition, 7-tesla T2-weighted FLASH discovered 604 cerebral lesions in the patients with relapsing-remitting MS, with a mean of 30.2 lesions per patient. No lesions were discovered among the healthy controls.
Cortical pathology was visible in 10 patients, with the detection of six cortical lesions and 37 leukocortical lesions. Within the 7-tesla acquisitions, each lesion detected at T2-weighted sequences was also visible on corresponding MP-RAGE sequences in the side-by-side analysis. At 1.5-tesla MRI, the MP-RAGE images found only 452 of 561 lesions (80%) in T2-weighted sequences.
The 7-tesla MP-RAGE sequence was also beneficial regarding the 217 T1 hypointense lesions detected in the MS subgroup. The images showed that each lesion persisted without major change in formation or size for at least one year, and could be classified as a black hole.
T1-weighted MP RAGE at 7 tesla is "highly sensitive" in detecting multiple sclerosis plaques within white and gray brain matter, and the technique depicted structural damage in each lesion, Sinnecker and colleagues concluded.
"To our knowledge, the present study is the first to demonstrate that, at ultrahigh-field strength, every T2 hyperintense lesion detected on T2-weighted FLASH sequences directly corresponds to a T1 hypointense lesion on a[n] MP-RAGE sequence," the authors wrote. "Our finding challenges previous studies, as well as our own data obtained at 1.5-tesla MRI, in which only 80% of T2 ... or hyperintense lesions were visible on MP-RAGE images."
Editor's note: The thumbnail on our homepage is a 7-tesla image of a glioblastoma patient. The T2-weighted image shows a brain lesion with very high spatial resolution. The heterogeneity in the lesion is already visible. Image courtesy of Dr. Michael Bock, medical physicist, Universitätsklinikum Freiburg, Freiburg, Germany.