VIENNA - Dynamic contrast-enhanced MR mammography is a sensitive method for detecting breast cancer because it highlights tumor vasculature, but diagnostic results may vary widely depending on reader experience. Diffusion-weighted imaging (DWI) and MR spectroscopy (MRS) aim to address this issue, and are continuing to show promise.
The neoplastic vasculature is induced in a mostly preclinical stage of breast cancer (2-3 mm in size). Consequently, MRI can detect these early breast cancers, which might be detected only by chance using conventional mammography because no mass or microcalcifications are present, said Dr. Pascal Baltzer, director of mammography at the Institute for Diagnostic and Interventional Radiology at Friedrich Schiller University in Jena, Germany. He will speak at today's breast refresher course on MRI diffusion, perfusion, and spectroscopy.
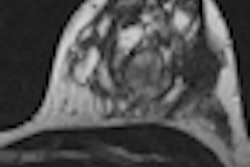
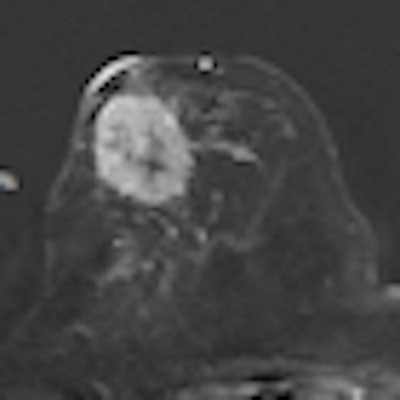
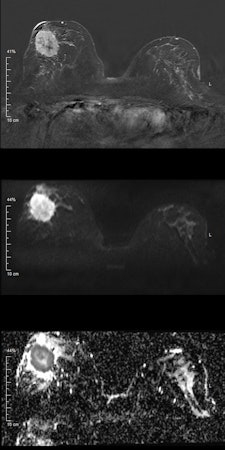 Invasive ductal carcinoma. Top: Early contrast-enhanced T1-weighted subtraction image depicting a large mass lesion in the right breast. Middle: Diffusion-weighted image at b = 1000 s/mm2 shows high signal corresponding to the contrast enhancement in the first image. However, in this case, the signal is due to restricted diffusion, meaning that no external contrast agent was used. Bottom: Quantitative parametric diffusivity map of apparent diffusion coefficient (ADC) values. Dark pixels correspond to restricted diffusion, while bright pixels correspond to increased diffusion. In the outer part of the tumor, dense clusters of cancer cells cause restricted diffusion; the diffusion measured by DWI is mainly caused by extracellular diffusion. Clearly, diffusivity is elevated inside the center of the lesion, corresponding to necrosis, which is indicative of a very aggressive cancer. All images courtesy of Dr. Pascal Baltzer.
Invasive ductal carcinoma. Top: Early contrast-enhanced T1-weighted subtraction image depicting a large mass lesion in the right breast. Middle: Diffusion-weighted image at b = 1000 s/mm2 shows high signal corresponding to the contrast enhancement in the first image. However, in this case, the signal is due to restricted diffusion, meaning that no external contrast agent was used. Bottom: Quantitative parametric diffusivity map of apparent diffusion coefficient (ADC) values. Dark pixels correspond to restricted diffusion, while bright pixels correspond to increased diffusion. In the outer part of the tumor, dense clusters of cancer cells cause restricted diffusion; the diffusion measured by DWI is mainly caused by extracellular diffusion. Clearly, diffusivity is elevated inside the center of the lesion, corresponding to necrosis, which is indicative of a very aggressive cancer. All images courtesy of Dr. Pascal Baltzer.
In investigations involving MRI techniques, pharmacokinetic modeling of high temporal resolution dynamic contrast-enhanced imaging (perfusion imaging) has promised quantitative insights into the pathological characteristics of neoplastic vasculature, while DWI and MRS are based on entirely different concepts.
"While MRS is a molecular imaging technique able to quantify biochemical tissue properties, DWI is influenced by microstructural tissue changes," he explained.
Baltzer plans to elaborate on implementing these techniques in clinical practice and the possible diagnostic benefits. A key benefit of using DWI or MRS is that no contrast agent is needed, unlike the regular MR mammography technique. DWI provides insight into subcellular tissue microstructure that is altered by neoplastic growth. Using MRS, chemical tissue components can be analyzed.
"Both techniques are promising, because they provide quantitative, and thus objective, information about target regions," he remarked. "However, DWI is far easier to implement into clinical practice as MRS is technically challenging and less easy to interpret."
DWI and MRS are additional techniques for tissue characterization, but their superiority over conventional mammography has not been demonstrated empirically, he stated. Moreover, perfusion, DWI, and MRS are, to different degrees, still investigational methods that cannot be recommended without caution for clinical practice, especially MRS.
Today's course is likely to interest both breast radiologists and oncologic radiologists because the techniques are not restricted to breast imaging.
"There is an ongoing trend toward noncontrast MRI techniques not only for breast cancer detection and lesion differentiation, but also for monitoring response to neoadjuvant treatment," Baltzer said. "Just recently, researchers at the DKFZ (Deutsches Krebsforschungszentrum) in Heidelberg have published a rapid communication on chemical exchange saturation transfer (CEST) imaging of the breast, which is another interesting MRI technique. The first PET/MR scanners may change our view on nuclear medicine in the role of breast cancer diagnosis. Furthermore, 3-tesla MRI is more broadly used for breast MRI, promising higher signal to noise, probably at the cost of challenging artifacts."
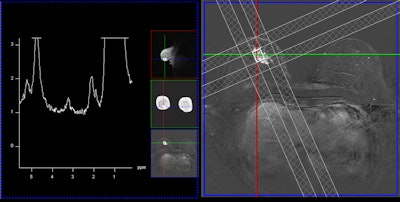 A single-voxel 1.5-tesla spectroscopy image of an invasive lobular carcinoma. The left image depicts the spectrum, i.e., the chemical components of the cancer, and the peak in the middle at about 3.23 ppm is due to tumor-specific choline metabolites. The right image shows the measurement voxel inside a contrast-enhancing mass (the cancer).
A single-voxel 1.5-tesla spectroscopy image of an invasive lobular carcinoma. The left image depicts the spectrum, i.e., the chemical components of the cancer, and the peak in the middle at about 3.23 ppm is due to tumor-specific choline metabolites. The right image shows the measurement voxel inside a contrast-enhancing mass (the cancer).Another presenter at the session, Dr. Alexandra Athanasiou from the department of radiology at the Institut Curie in Paris, will discuss ultrasound elastography, which maps breast lesion stiffness.
There are two elastography techniques available: strain imaging and shear-wave imaging. Strain imaging uses external compression gradually applied to the lesion by means of the ultrasound probe, deforming the lesion. In shear-wave imaging, no external compression is applied, and the ultrasound system induces mechanical vibration by using shear-wave imaging.
"The choice depends on the equipment and experience of each radiologist," stated Athanasiou, adding there is a slight advantage for shear-wave imaging because the radiologist can have absolute elasticity values whereas in strain imaging the radiologist obtains a semiquantitative lesion-fat value ratio.
Radiologists should always combine elastography with B-mode ultrasound because it can improve specificity and accuracy for BI-RADS lesions and potentially reduce breast biopsy rates, she added. However, elastography is useful mainly for indeterminate BI-RADS 4 and probably benign BI-RADS 3 lesions. For BI-RADS 3 lesions, elastography can help identify complicated cysts and reduce fine needle aspiration rates. It can also indicate a biopsy, instead of follow-up, in the case of BI-RADS 3 lesions with suspicious elastography findings.
"In BI-RADS 5 cancer cases, this technique may be helpful for characterizing additional lesions," she said.
During the course, Athanasiou will speak about the physics of elasticity imaging in a "radiology-friendly" manner, and clinical applications will be discussed so everyone feels comfortable about including this easy-to-perform technique in their everyday practice. Future trends include 3D elastography, as well as the use of ultrasound elastography in monitoring the response to neoadjuvant chemotherapy in women presenting with breast cancer, she concluded.
Originally published in ECR Today March 1, 2012.
Copyright © 2012 European Society of Radiology