Cardiac MR outperformed electrocardiography (ECG) for detecting unrecognized myocardial infarctions (MIs), catching many that were missed on ECG studies, according to a study published in the September 5 issue of the Journal of the American Medical Association.
In a group of 936 participants, cardiac MR detected 157 (17%) unrecognized myocardial infarctions, compared with 46 (5%) discovered with ECG, wrote lead author Dr. Erik Schelbert, director of cardiovascular MR at the University of Pittsburgh's Cardiovascular Institute, and colleagues.
"Although the prevalence of [unrecognized myocardial infarction] by ECG was similar to that in prior population studies, ECG was much less sensitive for detecting [unrecognized myocardial infarction] than cardiac MR," the authors wrote. "Prior population studies probably underestimate the prevalence of MI and particularly [unrecognized myocardial infarction] because they relied on ECG for detection." (JAMA, September 5, 2012, Vol. 308:9, pp. 890-897).
ICELAND MI study
The researchers analyzed older diabetic and nondiabetic individuals who were enrolled from January 2004 to January 2007 in ICELAND MI, a substudy of the Age, Gene/Environment Susceptibility-Reykjavik Study (AGES-Reykjavik), which since 1967 has followed men and women born in Iceland between 1907 and 1935.
Determining the prevalence of unrecognized myocardial infarction in the patient population is "relevant because age and diabetes increase the risks of coronary heart disease," the authors noted.
Participants were considered to have a recognized myocardial infarction when a history of MI was supported by hospital records. An unrecognized myocardial infarction by ECG was defined as having evidence of myocardial infarction by ECG criteria. Unrecognized myocardial infarction by cardiac MR meant there was no prior myocardial infarction based on hospital records.
The researchers also noted characteristics including the participants' demographics, risk factors related to atherosclerosis, other comorbidities, biochemical measurements from blood, and coronary calcium.
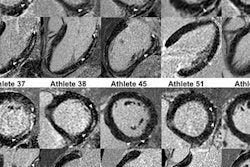
All 936 participants underwent cardiac MR scans on a 1.5-tesla scanner (GE Healthcare) using a four-element cardiac phased-array coil. The patients' median age was 76 years (range, 68 to 94 years), and there were 484 women (52%) and 452 (40%) men. Survivors were followed for a median of 6.6 years, ranging from 4.6 to 7.7 years.
Cardiac MR detection
Cardiac MR detected 91 (10%) participants with recognized myocardial infarctions and 157 (17%) with unrecognized myocardial infarction, Schelbert and colleagues wrote. Cardiac MR also detected more unrecognized myocardial infarction in diabetic individuals than ECG (21% versus 4%).
ECG found 27 participants (3%) with unrecognized myocardial infarction who exhibited no myocardial infarction on cardiac MR. There were 138 patients (15%) who had unrecognized myocardial infarction by cardiac MRI yet did not meet the criteria for unrecognized myocardial infarction by ECG.
In the randomly sampled cohort (670 participants), 61 (9%) had recognized myocardial infarctions and 97 (14%) had unrecognized myocardial infarction by cardiac MR; in contrast, only 35 subjects (5%) had unrecognized myocardial infarction by ECG.
Risk factors
The group also found that coronary artery disease risk factors were more prevalent in participants with unrecognized MI than in those with no myocardial infarction.
Those with unrecognized myocardial infarction were more often male, slightly older, and had more hypertension and diabetes, the authors wrote. In addition, subjects with unrecognized myocardial infarction had more atherosclerosis and significantly higher coronary calcium scores than those with no evidence of MI.
Over a median follow-up of 6.4 years, 30 (33%) of 91 participants with recognized MI died and 44 (28%) of 157 subjects with unrecognized MI as seen by cardiac MR died. These rates were significantly higher than the 119 (17%) of 688 individuals with no myocardial infarction who died, according to the authors.
In conclusion, the researchers noted that older individuals had a higher prevalence of myocardial infarction, especially those with diabetes, and most MI were unrecognized, despite the association with atherosclerosis and other risk factors.
Cardiac MR detected more unrecognized myocardial infarction and was more strongly associated with mortality than ECG, they stated.


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)