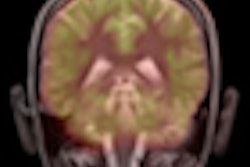
Researchers trying to develop better tools for predicting who will develop Alzheimer's disease used MRI to detect bright areas in the brain that indicate small-vessel cerebrovascular disease. The technique could be used with PET scans of beta-amyloid levels to predict Alzheimer's, according to a February 18 study in JAMA Neurology.
The group from Columbia University Medical Center believes that the bright areas, called white-matter hyperintensities, are signs of small-vessel cerebrovascular disease and part of the clinical presentation of Alzheimer's. Detection of the areas could offer additional information that complements PET scans of beta-amyloid levels, which aren't 100% certain in predicting which patients will eventually develop Alzheimer's.
The study was led by Frank Provenzano from Columbia's Taub Institute for Research on Alzheimer's Disease (JAMA Neurology, February 18, 2013).
Drawbacks of beta amyloid
Previous research has shown an association between beta-amyloid deposits in the brain and Alzheimer's disease, according to the authors. However, autopsy studies have also found that as many as 30% of older individuals with no symptoms of Alzheimer's have the same elevated beta-amyloid levels as people with the disease.
Furthermore, the amount of measurable beta-amyloid deposits is a "relatively weak correlate" of symptom severity among individuals with Alzheimer's or those at risk for Alzheimer's. "Together, these findings suggest that beta amyloid is necessary but perhaps not sufficient to cause the syndrome associated with the disease," the authors wrote.
Provenzano and colleagues used data from the Alzheimer's Disease Neuroimaging Initiative (ADNI) to study 21 normal control subjects, 59 individuals with mild cognitive impairment, and 20 people with Alzheimer's.
The information included participants' PET scans with carbon-11-labeled Pittsburgh Compound B (PiB) to determine PiB-positive subjects, and/or confirm the presence of significant beta-amyloid deposits.
Of the 41 scans from patients with Alzheimer's disease and the control subjects, 28 individuals (68%) were classified as PiB-positive. Of those 28 subjects, 11 were classified as normal and the remaining 17 were clinically defined as having Alzheimer's.
Of the scans from the 59 subjects with mild cognitive impairment, 41 participants (69%) were PiB-positive. In addition, 13 PiB-negative participants were deemed to have Alzheimer's.
The researchers then investigated the utility of MRI in the study group to compare the results with PiB-PET images. Because MRI can illustrate small-vessel cerebrovascular disease as brightly lit white-matter hyperintensities, the researchers collected T1-weighted, T2-weighted, and proton density MRI sequence information on the study participants.
MRI scans were acquired within six months of the PiB-PET images, and total white-matter hyperintensity (WMH) volume was calculated for each subject. The mean total WMH volume was 5.71 cm3 (median, 2.27 cm3), and total WMH volume did not differ between PiB-positive and PiB-negative individuals.
WMH volume
Among subjects who were positive on the PiB-PET studies, the researchers found increased WMH volume for those with an Alzheimer's diagnosis. Based on a cutoff of 1.25 cm3 total WMH volume, sensitivity was 83% and specificity was 64% in determining which participants had Alzheimer's.
The researchers also followed participants with mild cognitive impairment for a mean 29.7 months and a median 35 months from the time of their initial evaluation to their Alzheimer's diagnosis or last available follow-up assessment. Of the 59 subjects with mild cognitive impairment, 22 (37%) converted to Alzheimer's during the follow-up interval.
Based on the results, Provenzano and colleagues concluded that the severity of white-matter hyperintensities and beta-amyloid deposits on PiB-PET scans were independently associated with an Alzheimer's diagnosis.
In addition, among subjects with amyloidosis, WMH volume was able to differentiate between Alzheimer's cases and normal control subjects with "excellent sensitivity and good specificity," the authors noted. Both PiB and WMH status also were "significant predictors" of which people with mild cognitive impairment would progress to Alzheimer's.
"The findings suggest a role of small-vessel cerebrovascular disease in the clinical presentation of Alzheimer's and point to the importance of incorporating WMH into the formulation of pathogenic models of the disease," the authors wrote.
The findings are preliminary and larger studies are needed to confirm the conclusions, Provenzano and colleagues noted.
"Regardless of mechanistic associations between WMHs and Alzheimer's pathology, it is becoming clear from studies, such as this one and others, that vascular factors are quite important in the pathogenesis of the Alzheimer's phenotype, which suggests clinical strategies for disease prevention and treatment," they concluded.