When used as an adjunct to mammography and ultrasound, MRI can find additional cancers and provide more detail about their location in patients with breast implants, according to a study from Memorial Sloan-Kettering Cancer Center.
MR images also showed that breast cancer is often in contact with the implant or the pectoralis muscle, and a tumor can spread along an implant's contour, with the pectoralis at risk from the invading cancer.
In the study, the modality visualized cancer that was missed by mammography or ultrasound in 16 (30%) of 54 cases, noted lead study author Dr. Victoria Mango, an assistant professor of clinical radiology at Columbia University Medical Center.
Limited information
"Imaging appearance of breast carcinoma in patients with augmentation has been characterized on mammography and ultrasound, but there is limited information about MRI appearance," Mango said during her presentation of the results at last week's American Roentgen Ray Society (ARRS) meeting.
Mango and colleagues culled the 54 patients with breast implants from the MRI database at Memorial Sloan-Kettering. All of the women had biopsy-proven breast carcinoma on their MRI exams between 2000 and 2010.
One breast radiologist evaluated the images, looking at implant type and location; imaging characteristics of the carcinoma, such as size, enhancement pattern, and its relationship to the implant and pectoralis; lymph node disease; and other MRI findings.
The researchers also collected information such as patient age, the date of breast augmentation, how the patient presented clinically, and the tumor and node pathology.
The median age at diagnosis was 49 years, with a range of 28 to 72 years. Thirty-eight participants (70%) had cancers that were palpable. Implants were in place for a mean of 10 years (range, 0.3-35 years) prior to diagnosis. Thirty-one women (57%) had saline augmentation, 22 (41%) had silicone implants, and one (2%) had an inner silicone/outer saline implant.
Mean tumor size was 2.8 cm, ranging from 0.6 cm to 9.6 cm, according to the group. There were 46 (85%) invasive cancers, including 35 invasive ductal carcinomas, seven invasive lobular carcinomas, and four with mixed features, along with eight cases (15%) of ductal carcinoma in situ.
The researchers were able to identify adenopathy, or enlargement of the lymph node, on MRI in eight patients. The lymph nodes were positive at pathology for 18 (30%) of 48 cases with nodal information available.
Mango and colleagues also saw mass enhancement in 34 patients (63%). Thirty tumors had irregular shape and 34 had noncircumscribed margins, while 22 showed heterogeneous internal enhancement and 12 had rim enhancement. The remaining 20 patients (37%) had nonmass enhancement.
"There was no appreciable difference between implant position and lesion morphology or tumor size," the researchers noted.
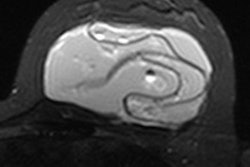
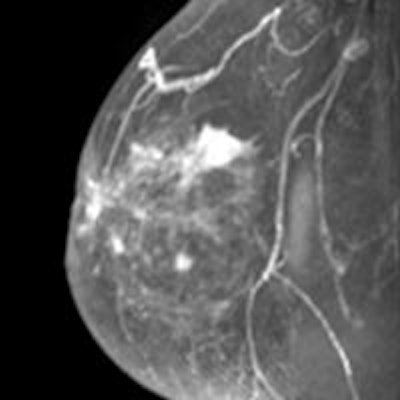
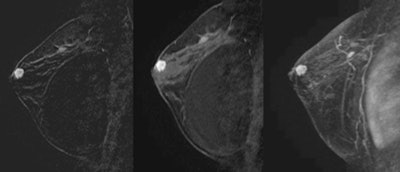 MRI of a 38-year-old woman with saline implants for two years and a family history of breast cancer. The patient had a palpable mass with a negative mammogram; guided biopsy yielded invasive ductal carcinoma. All images courtesy of Dr. Victoria Mango.
MRI of a 38-year-old woman with saline implants for two years and a family history of breast cancer. The patient had a palpable mass with a negative mammogram; guided biopsy yielded invasive ductal carcinoma. All images courtesy of Dr. Victoria Mango.One of the more noteworthy findings, Mango said, was the relationship of the cancers to the implant and the pectoralis muscles.
"In 20 of these cases, the cancers actually abutted the implant," she said. "In 18 of those 20, the cancer spread along the implant capsule for greater than 5 cm."
That finding was more common among retroglandular implants (nine of 16 patients, or 56%) than among retropectoral implants (nine of 38 patients, or 24%). In retropectoral implants, the tumor appeared to contact the implant where it was not covered by the pectoralis muscle.
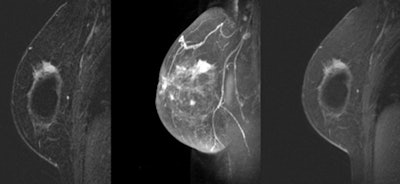 MRI shows an invasive ductal carcinoma abutting an implant in a 58-year-old woman with a palpable mass and retroglandular saline implants for 30 years. There is a spiculated mass abutting the superolateral implant. An outside mammogram and ultrasound failed to show the carcinoma.
MRI shows an invasive ductal carcinoma abutting an implant in a 58-year-old woman with a palpable mass and retroglandular saline implants for 30 years. There is a spiculated mass abutting the superolateral implant. An outside mammogram and ultrasound failed to show the carcinoma.Breast MRI also found 13 cancers (24%) abutting the pectoralis muscle, with eight paralleling the muscle contour. Two cancers (4%) invaded the pectoral muscle.
As for MRI's overall benefit, the modality was able to visualize cancer in 16 cases in which it was not seen on mammography or ultrasound. In five cases, tumor size was larger with MRI than on mammography and ultrasound. For 12 individuals, MRI found multicentric disease that was not seen on mammography or ultrasound.
"In this group, we had 12 additional biopsies performed, not including the index cancers, seven of which were benign and five malignant," Mango added.
She cited several limitations of the study, including the small number of patients, the fact that it was a single-reader retrospective review, and that the MRI exams took place over a 10-year period during which there were differences in breast MRI technique.
In conclusion, Mango said that MRI "may be a valuable adjunct in this patient population, particularly for evaluating the extent of disease and occult contralateral carcinoma, but we did see a limited identification of nodal disease."