Functional MRI (fMRI) scans of the brain at rest show disruptions in neural networks in patients with early Alzheimer's disease at about the same time as chemical markers of the disease begin to appear in cerebrospinal fluid, according to a study published online August 19 in JAMA Neurology.
The researchers from Washington University in St. Louis assessed resting-state brain fMRI along with the presence of beta-amyloid plaque and tau protein in the cerebrospinal fluid to detect the early onset of Alzheimer's disease.
The findings are among the first to show how resting-state fMRI may be an equally effective and less invasive way to detect early development of the disease, according to Dr. Liang Wang, from the department of neurology, and colleagues.
Early markers of Alzheimer's
Previous research has shown that Alzheimer's patients accumulate beta-amyloid plaque and tau proteins in the brain years before Alzheimer's appears, the authors wrote. Different levels of these two markers in the spinal fluid are considered reliable indicators of preclinical Alzheimer's.
In addition, as a noninvasive way to evaluate the neural network, resting-state functional connectivity MRI has "considerable potential" for the detection of preclinical Alzheimer's, according to Wang and colleagues.
Early diagnosis of Alzheimer's is a priority because many physicians believe that treating patients long before dementia appears will greatly improve patient outcome.
In the current study, Wang and colleagues took multiple samples of spinal fluid over several years from 207 older but cognitively normal volunteers at the Charles F. and Joanne Knight Alzheimer's Disease Research Center at Washington University. The researchers analyzed the samples for changes in both beta amyloid and tau protein (JAMA Neurology, August 19, 2013).
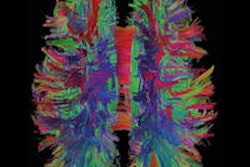
The participants were also imaged repeatedly on a 3-tesla MRI system (Trio, Siemens Healthcare). They were instructed to concentrate on a visual crosshair, remain still, and not fall asleep during the scanning. With this resting-state fMRI, the researchers were able to track the rise and fall of blood flow in different brain regions.
Default mode network
The data were used to assess the integrity of the brain's default mode network, which is a set of connections between different regions that becomes active when the mind is at rest. Earlier studies by Wang, senior author Dr. Beau Ances, PhD, and other researchers have shown that Alzheimer's disease damages connections in the default mode network, as well as in other brain networks.
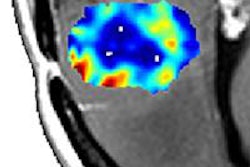
In this study, fMRI was able to detect damage at about the same time that beta-amyloid deposits began to increase and tau levels started to decrease in spinal fluid. The part of the default mode network most harmed by the onset of Alzheimer's disease was the connection between the posterior cingulate and medial temporal regions, which are areas of the brain associated with memory.
The effects of beta amyloid and tau protein in cerebrospinal fluid, "each of which independently affected default mode network functional connectivity, were not attributable to age or structural atrophy in the posterior cingulate cortex and the medial temporal lobe," the authors wrote.
Based on the results, Wang and colleagues concluded that the "convergent effects" of decreased beta amyloid and increased tau on the brain's default mode network "provide insights into the early pathogenesis" of Alzheimer's disease.
The data "suggest that memory impairment in the early phases of Alzheimer's disease may be attributable to the convergent effects of both amyloid and tau pathology," the researchers noted.
Wang and colleagues plan to continue their research into the connections between brain network damage and the progress of early Alzheimer's disease in normal volunteers and in patients in the early stages of Alzheimer's-associated dementia.
"Further work is warranted to examine the effects of cerebrospinal-fluid biomarker abnormalities in resting-state networks other than the default mode network," they wrote.
Study disclosures
The study received funding from several sources, including the U.S. National Institute of Neurological Disorders and Stroke, the National Institute of Mental Health, the National Institute on Aging, the American Roentgen Ray Society, the National Institute of Nursing Research, and the Alzheimer's Association.