Abnormalities throughout the spinal cord and the number of segments affected by spinal cord lesions are the most significant MRI parameters for characterizing physical disabilities caused by multiple sclerosis (MS), according to a study published in the November issue of Radiology.
Researchers from St. Josef Hospital in Bochum, Germany, also found that the number of spinal cord segments affected by MS, as seen on MRI, especially in the upper cervical cord cross-sectional area (UCCA), are associated with walking abilities. For patients with MS, the findings confirm how spinal cord abnormalities affect their ambulatory function.
Lead author is Dr. Carsten Lukas from the hospital's department of diagnostic and interventional radiology and nuclear medicine (Radiology, November 2013, Vol. 269:2, pp. 542-552).
MRI lacks specificity?
While newer imaging modalities have improved the detection of spinal cord lesions in multiple sclerosis patients, previous studies also have shown that conventional MRI lacks specificity in this application, prompting the need for other quantitative techniques, such as measurement of spinal cord atrophy, to evaluate MS patients.
The current study retrospectively evaluated 440 MS patients (287 women, 153 men) from two medical centers between May 2004 and December 2007. Among the participants were 311 people with relapsing-remitting MS, 92 cases of secondary-progressive MS, and 37 patients with primary-progressive MS.
MRI exams were performed on 1.5-tesla systems at both facilities (Magnetom Vision, Magnetom Avanto, Siemens Healthcare) through which researchers measured the UCCA, brain and spinal cord lesions, and brain atrophy for all subjects. In addition, the number of lesions was determined through contrast-enhanced T1-weighted MRI.
MR images of the entire spinal cord were available for 420 patients and were used to tally the number of focal lesions, spinal segments affected by MS, and the presence of diffuse abnormalities. Diffuse abnormalities were defined as areas with greater signal intensity than that of cerebrospinal fluid in the spine.
The researchers also evaluated correlations between the UCCA and clinical and other MRI parameters, including the number of brain lesions on T1-weighted MRI, presence of diffuse abnormalities, and number of segments in the spinal cord affected by MS. In addition, they analyzed normalized brain volume based on head size, normalized gray-matter volume, and normalized white-matter volume.
MRI parameters
MR images revealed the presence of spinal cord lesions in 312 (74.3%) of the 420 patients, while 438 (99.5%) of the participants had abnormalities seen on the T2-weighted brain MR images. Diffuse spinal cord abnormalities also were evident in 61 (14.5%) of the 420 patients. A median of two spinal cord lesions were found per patient, while the median number of segments affected by MS was 1.75.
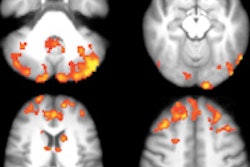
 Sagittal T2-weighted (A) and proton density-weighted (B) MR images of the spinal cord in a 45-year-old woman with 13 years of primary-progressive MS. Diffuse hyperintensity shows diffuse abnormalities of the entire spinal cord (*) and is best seen on corresponding proton density-weighted image. Image courtesy of Radiology.
Sagittal T2-weighted (A) and proton density-weighted (B) MR images of the spinal cord in a 45-year-old woman with 13 years of primary-progressive MS. Diffuse hyperintensity shows diffuse abnormalities of the entire spinal cord (*) and is best seen on corresponding proton density-weighted image. Image courtesy of Radiology.
The researchers also found the number of spinal cord lesions and the number of involved segments in the spinal cord were significantly higher among secondary-progressive MS patients, compared with relapsing-remitting MS cases. They found no significant difference between the other disease types.
Scattered abnormalities also were found more frequently among the chronic disease types, with the highest frequency in patients with primary-progressive MS.
In addition, UCCAs in patients with secondary-progressive MS and primary-progressive MS were significantly smaller than those in patients with relapsing-remitting MS. The group found no significant difference in the UCCAs of patients with secondary-progressive MS compared with individuals with primary-progressive MS.
The UCCA did significantly correlate with brain MRI parameters among the study participants and was most significantly associated with brain atrophy measures based on normalized brain volume, normalized white-matter volume, and a normalized gray-matter volume.
The association between those brain atrophy measures and the UCCA suggests that "brain and spinal cord atrophy proceed hand in hand, to some degree," the authors wrote. "Interestingly, the presence of enhancing brain lesions was also associated with UCCA, which suggests that the spinal cord cross-sectional area is larger during acute inflammation."
Based on the findings, Lukas and colleagues concluded that the UCCA, scattered abnormalities in the spinal cord, and the number of segments affected by spinal cord lesions are the most significant MRI parameters for explaining physical disabilities caused by MS.
"Furthermore, the number of involved spinal cord segments and especially UCCA were associated with walking abilities," they wrote, "Which confirms the importance of spinal cord abnormalities with regard to ambulatory dysfunction in MS."