
Using MRI to image carotid artery plaque can accurately predict future cardiovascular events such as strokes and heart attacks in people with no history of cardiovascular disease, according to a new study published online March 4 in Radiology.
The researchers from Canada and the U.S. found that the presence of a lipid core in the internal carotid artery on MRI was a significant predictor of subsequent adverse events. MRI also improved the prediction of future cardiovascular events compared to traditional risk factors alone.
This is the first population-based prospective study to determine if vulnerable plaque features by MRI add to the risk of a cardiovascular event beyond the traditional risk factors, according to study senior author Dr. David Bluemke, PhD, director of radiology and imaging sciences at the National Institutes of Health (NIH) Clinical Center, in a statement from RSNA.
Versatile modality
The new study demonstrates MRI's versatility in determining the risk of future adverse events, particularly in individuals who do not seem at risk.
"MRI is unique in that it is one of the few ways to see if one of these subcomponents of plaque is present at all," Bluemke told AuntMinnie.com. This study was "specifically designed to look at people who are relatively normal, follow them for a very long period of time, and then determine which factors help us predict who is at risk for severe events."
Previous research has shown that some arterial plaque is more dangerous because of its vulnerability to rupture. MRI can discern features of this vulnerable plaque, such as a lipid core with a thin fibrous cap, making MRI potentially valuable for identifying patients at risk for future cardiovascular events.
"We previously did not know if these plaque features were more or less incidental, or if they are actually critical in terms of our understanding someone's risk for a cardiovascular event," Bluemke said.
MESA enrollment
Participants in the current study came from the Multi-Ethnic Study of Atherosclerosis (MESA), which included 6,814 adults between the ages of 45 and 84 who had no cardiovascular disease at the time of enrollment between July 2000 and September 2002. The participants were categorized according to gender and ethnicity at six different facilities in the U.S., wrote lead author Dr. Anna Zavodni, from the University of Toronto's Sunnybrook Health Sciences Centre, and colleagues (Radiology, March 4, 2014).
Zavodni's group used ultrasound to assess carotid wall thickness and MRI to define carotid plaque composition and remodeling index, a measure of changes in vessel size, in 946 asymptomatic patients from MESA. Each MESA center used a 1.5-tesla MRI scanner and dedicated carotid coils to obtain images of the carotid arteries.
The researchers also measured cardiovascular events such as heart attack, resuscitated cardiac arrest, angina, stroke, and death in these asymptomatic patients over an average of 5.5 years.
Among people who have died or suffered an adverse cardiovascular event, certain subcomponents of atherosclerosis are evident when the artery is partially removed or autopsied, Bluemke said.
"One of the more histological components seems to be this lipid core," he explained. "In the area of the artery's thick wall, if the wall erodes, it exposes lipid core to the bloodstream and a clot will form. In a large vessel, such as the carotid artery, that clot can potentially break off, go to the brain, and cause a stroke."
Carotid artery plaque features have mostly been studied by MRI only when there was marked artery narrowing or after a patient had a stroke. "For the rest of the population, we really don't know if plaque features were significant or if the most significant factor is simply that there is a lot of thickening of that artery," he added.
Event predictors
Cardiovascular events occurred in 59 subjects (6%), the researchers found. Carotid intima-media thickness as determined by ultrasound and remodeling index, lipid core, and calcium in the internal carotid artery on MRI were all significant predictors of cardiovascular events in univariate analysis.
A lipid core was present in almost half of the patients who had an adverse event, compared with only 17.8% of participants who did not have an event, according to Zavodni and colleagues.
MRI was also useful in reclassifying baseline risk for cardiovascular events. When both the MRI remodeling index and lipid core were used to assess risk, 15.8% more patients with events and 7.4% without events were correctly reclassified compared to the use of traditional risk factors.
"Our results support the concept that adverse carotid arterial remodeling and a lipid core at MR imaging confer increased risk for subsequent cardiovascular events in asymptomatic individuals," the authors wrote.
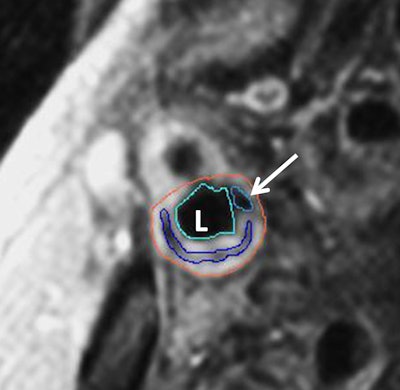
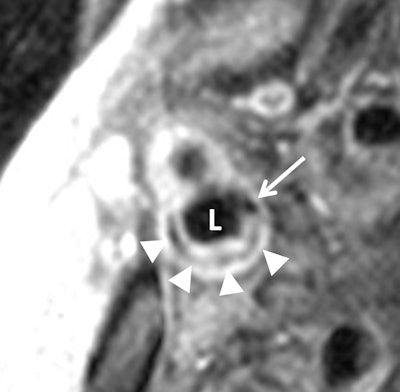 Transverse gadolinium-enhanced T1-weighted MR images show carotid artery bifurcation in a 72-year-old man. Above, low-signal-intensity calcium (arrow) and lipid core (arrowheads) can be seen in internal carotid artery (ICA) lumen (L). Contouring of the ICA is seen in the image below. The outer adventitial wall (orange), lipid core (purple), calcification (arrow), and vessel lumen (teal) are visible. Images courtesy of Radiology and Dr. David Bluemke, PhD.
Transverse gadolinium-enhanced T1-weighted MR images show carotid artery bifurcation in a 72-year-old man. Above, low-signal-intensity calcium (arrow) and lipid core (arrowheads) can be seen in internal carotid artery (ICA) lumen (L). Contouring of the ICA is seen in the image below. The outer adventitial wall (orange), lipid core (purple), calcification (arrow), and vessel lumen (teal) are visible. Images courtesy of Radiology and Dr. David Bluemke, PhD.
The findings "are really the first results in a large population that indicate the value of MRI in very early plaque disease," Bluemke added. "The plaque that has been studied before has been very advanced, when someone had had a stroke, heart attack, or postmortem. Our results indicate the high sensitivity of MRI for looking at these plaque features and tell us it is clinically significant when we see the plaque features."
However, while MRI is the "most sensitive test" for this application, the modality is expensive, Bluemke noted. Today's ultrasound and CT technologies are much more sensitive than in the past and are viable alternatives for screening, especially with improvements in CT dose reduction.
Yet "MRI is the noninvasive way that provides images of the artery wall in addition to the components of the wall," Bluemke said. "By comparison, ultrasound primarily is used to find the thickness of the wall and the extent of narrowing. CT will provide some calcification in the wall, but it cannot characterize the wall as accurately as MRI."
The researchers plan to follow this patient population for at least another five years to assess other measures such as calcium score.
"In addition, we and other centers are looking at ways to reduce the plaque in the artery," Bluemke said. "When we can reduce the plaque, perhaps with a statin therapy, we would look to see if the lipid core within the plaque will be reduced."




















