Prostate cancer biopsy with a targeted technique that fuses MR and ultrasound images outperformed traditional extended-sextant ultrasound-guided biopsy, identifying more high-risk cancers and fewer low-risk malignancies, according to research published in the January 27 issue of the Journal of the American Medical Association.
In a prospective study of more than 1,000 men who received both methods concurrently, a research team from the U.S. National Cancer Institute (NCI) found that the targeted biopsy method diagnosed nearly one-third more high-risk cancers while identifying almost one-fifth fewer lower-risk cancers.
"This study demonstrated that targeted biopsy could significantly change the distribution of risk in men newly diagnosed with prostate cancer toward diagnosis of more high-risk disease," wrote the group led by Dr. Mohummad Minhaj Siddiqui, now at the University of Maryland School of Medicine.
Finding more higher-risk cancer
Prostate cancer has traditionally been detected by standard extended-sextant biopsy, which involves random sampling of the entire prostate. Thanks to the development of multiparametric MRI, however, imaging-based identification of prostate cancer shows potential for bolstering diagnostic accuracy for higher-risk tumors, according to the researchers (JAMA, January 27, 2015, Vol. 313:4, pp. 390-397).
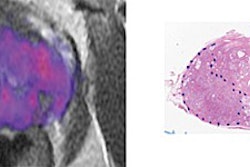
At the same time, targeted MR/ultrasound fusion biopsy platforms have been introduced to allow multiparametric MR images to be superimposed in real-time on transrectal ultrasound images. While earlier trials of these targeted biopsy techniques had found the combination of targeted biopsy with standard biopsy to be superior to standard biopsy alone, the results sparked questions about whether standard biopsy was still necessary, the authors wrote.
As a result, the group sought to directly compare the two techniques independently and in combination for diagnosing intermediate-risk to high-risk prostate cancer. As part of an ongoing National Institutes of Health (NIH) study on the use of electromagnetic tracking devices to locate disease during multimodality-navigated procedures, patients were enrolled in a prospective clinical trial between August 2007 and February 2014 at NCI in Bethesda, MD.
Men were included in the study if they had an elevated prostate-specific antigen test or an abnormal digital rectal examination as well as a multiparametric MRI finding of at least one prostate lesion. Patients with prior prostate cancer therapy or a contraindication to multiparametric MRI were excluded from the study.
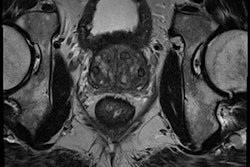
Multiparametric MRI was performed using an Achieva 3-tesla scanner (Philips Healthcare) with a Sense 16-channel surface coil (Philips) and BPX-30 endorectal coil (Bayer HealthCare). Four sequences were used: triplanar T2-weighted, dynamic contrast-enhanced, diffusion-weighted imaging, and MR spectroscopy.
Two genitourinary radiologists with eight and 14 years of experience in interpreting prostate multiparametric MRI studies independently reviewed and formed consensus reads of all of the exams. They assigned scores to indicate suspicion, rating lesions as either low, moderate, or high based on previously described criteria.
DynaCAD software (Invivo) was then used to segment lesions and record their location prior to biopsy. After receiving a targeted biopsy performed by one physician with a UroNav MR/ultrasound fusion device (Invivo), another physician who was not aware of the MR lesion locations performed a standard biopsy. An end-fire transrectal ultrasound probe (Philips) was used to sample lesions in both axial and sagittal planes, according to the researchers.
Differences in detection
Of the 1,003 men included in the study, targeted biopsy detected cancer in 461 patients, compared with 469 with standard biopsy. While the methods agreed exactly in 690 men (69%), they differed in the remaining cases.
| Targeted vs. standard biopsy for prostate cancer | ||
| Diagnosis of high-risk cancers | Diagnosis of low-risk cancers | |
| Targeted biopsy | 173 cases | 213 cases |
| Standard biopsy | 122 cases | 258 cases |
Targeted biopsy detected 30% more high-risk cancers and 17% fewer low-risk cancers, according to the team. The differences were statistically significant (p < 0.001 and p = 0.002, respectively).
In other findings, combining the two methods yielded limited utility; it would detect 103 more cancer cases (22%), but 83% of these were low-risk, 12% were intermediate-risk, and only 5% were high-risk, the researchers found.
"This equated to a number needed to biopsy with standard biopsy in addition to targeted biopsy of 200 men to diagnose one additional high-risk cancer," they wrote. "Furthermore, for every additional case of high-risk cancer diagnosed, 17 additional cases of low-risk cancer would be diagnosed."
They also noted that targeted biopsy's predictive ability for differentiating low-risk from intermediate- and high-risk disease in a subset of 170 men with whole-gland pathology after prostatectomy was higher than either standard biopsy or a combination of the two techniques.
The study shows that targeted biopsy could significantly alter the risk distribution in men newly diagnosed with prostate cancer toward diagnosis of more high-risk disease, the researchers concluded.
"Although these improvements in risk stratification could translate into substantial clinical benefits, it is important to recognize that this study is preliminary with regard to clinical end points such as recurrence of disease and prostate-cancer-specific mortality," they wrote. "These findings provide a strong rationale for the conduct of randomized clinical trials to determine the effect of targeted biopsy on clinical outcomes."