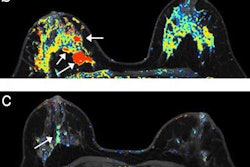
TORONTO - A new method of dynamic contrast-enhanced (DCE) MRI is an "excellent early predictor" of treatment response and a good marker of residual cancer burden during and after neoadjuvant chemotherapy for breast cancer, according to a study at the International Society for Magnetic Resonance in Medicine (ISMRM) meeting.
Even after only one round of neoadjuvant chemotherapy, changes in several quantitative biomarkers detected by the DCE-MRI approach provided "excellent predictions of eventual pathologic complete response or noncomplete response, potentially playing an important role in personalized care of breast cancer patients in the future," the researchers from Oregon Health and Science University wrote in a study abstract.
"We found that DCE-MRI can give us an early prediction of responders versus nonresponders, as DCE-MRI is one of the useful imaging tools to measure the microvascular properties within a tumor," lead author Alina Tudorica, PhD, an assistant professor of radiology, told AuntMinnie.com.
An urgent need
Neoadjuvant chemotherapy is being used more often to treat locally advanced breast cancer, which might allow for breast conservation surgery in patients with reduced cancer burden after treatment, the researchers noted.
 Alina Tudorica, PhD, from Oregon Health and Science University.
Alina Tudorica, PhD, from Oregon Health and Science University.Past research has shown that complete response to neoadjuvant chemotherapy is a strong indicator of survival. However, only a small percentage of patients turn out to be completely cancer-free, and under the current standard of care, response can only be determined after pathological examination of tissue specimens from postchemotherapy surgery.
"Thus, there is an urgent need for minimally invasive methods to provide early prediction of therapy response, potentially allowing rapid, personalized treatment-plan alteration for nonresponding patients," Tudorica and colleagues wrote.
In their study, the researchers measured microvascular properties of tumors using a standard pharmacokinetic model (SM) and a relatively new model of DCE-MRI referred to as the shutter-speed model (SSM). Developed at the university, shutter-speed MRI could be more sensitive than standard DCE-MRI protocols by taking into account the kinetics of cross cell membrane water exchange. DCE-MRI metrics include Ktrans, a measure of blood flow and vessel permeability, and τi, which is unique to the shutter-speed model and is a measure of cellular metabolic activity.
The research cohort consisted of 21 consecutive patients with locally advanced breast cancer who underwent neoadjuvant chemotherapy. DCE-MR images were acquired at four time points to assess tumor response: at the patient's first visit prior to neoadjuvant chemotherapy; after the first round of chemotherapy; at the midpoint of chemotherapy, usually after three treatment cycles; and after treatment completion.
MRI protocols
The researchers used a 3-tesla MRI scanner to acquire axial bilateral DCE-MR images with full breast coverage through a 3D gradient echo-based time-resolved angiography with stochastic trajectories (TWIST) sequence. Total image acquisition time was approximately 10 minutes for 32 to 34 image volume sets with 14- to 20-second temporal resolution. Subjects received an intravenous injection of the contrast agent gadoteridol (ProHance, Bracco Imaging), which was timed to start after acquisition of the first two baseline image volumes.
Experienced radiologists determined tumor regions of interest from the postcontrast DCE images and measured tumor size according to Response Evaluation Criteria in Solid Tumors (RECIST).
A patient's pathologic response to neoadjuvant chemotherapy and residual cancer burden were determined by analyzing resected specimens after treatment and comparing the results with core biopsy specimens taken for cancer diagnosis before neoadjuvant chemotherapy.
At the end of chemotherapy, Tudorica and colleagues determined that five patients had a complete pathologic response, with no invasive cancer cells found in resection specimens. The other 16 patients had a partial response, with reduced cancer cell density in resection specimens compared to biopsy samples taken prior to treatment.
The percentage changes in DCE-MRI parameters including Ktrans and τi after the first neoadjuvant chemotherapy cycle (visit No. 2 for MRI scanning) were "excellent early discriminators" of a complete or partial response, according to the researchers. The τi parameter had a statistical c-value (which is equivalent to area under the receiver operator characteristics [ROC] curve) of 0.938, indicating excellent prediction of response.
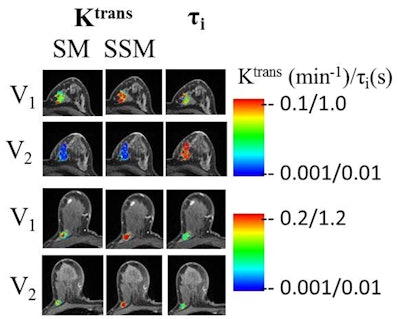 Two breast tumors before neoadjuvant chemotherapy (V1) and after one round of chemotherapy (V2). One subject was a pathologic complete responder (top two rows) and the other was a pathologic partial responder (bottom two rows). There was a substantial Ktrans decrease and τi increase after only one round of therapy in the complete responder compared to the noncomplete responder. Color bars indicate the coding of DCE-MRI biomarker values from small (blue) to large (red). Images courtesy of Alina Tudorica, PhD.
Two breast tumors before neoadjuvant chemotherapy (V1) and after one round of chemotherapy (V2). One subject was a pathologic complete responder (top two rows) and the other was a pathologic partial responder (bottom two rows). There was a substantial Ktrans decrease and τi increase after only one round of therapy in the complete responder compared to the noncomplete responder. Color bars indicate the coding of DCE-MRI biomarker values from small (blue) to large (red). Images courtesy of Alina Tudorica, PhD.By comparison, RECIST -- a standard-of-care method -- was a poor predictor of response, with a c-value of 0.619 after one round of chemotherapy, "though it is a valuable marker of residual cancer burden after neoadjuvant chemotherapy completion," the authors wrote.
The unique aspect of this study is the use of the τi biomarker as an added metabolic dimension of DCE-MRI for tumor response assessment.
"The ability of the DCE-MRI method to characterize synergistic microvascular perfusion and cellular energetic metabolism simultaneously may harbor great promise for studying tumor microenvironment, and its response to therapy," the group concluded.
Tudorica and colleagues plan to advance their research by validating these results with more patients.
"Because of the excellent performance of these DCE-MRI biomarkers for early prediction of breast cancer therapy response, it is very important to validate the initial results with more patients and maybe include multivariate analyses of the imaging biomarkers for even more accurate early prediction of therapy response," Tudorica said.