A shorter noncontrast-enhanced breast MRI protocol might help reduce the number of unnecessary biopsies by gathering additional information about suspicious lesions found on screening mammography while cutting scanning times, according to a new study published online September 29 in Radiology.
With a negative predictive value of 92%, the accuracy of the diffusion-weighted imaging with background suppression (DWIBS) protocol was comparable to that of conventional diagnostic MRI and an abbreviated contrast-enhanced protocol. In addition, images were obtained in approximately seven minutes using the DWIBS method, compared with more than 30 minutes for a standard full breast MRI protocol.
This abbreviated approach might help increase the rate of positive biopsies from current estimates of only 48% to 50% after suspicious screening mammograms to more than 90%, if all negative findings were considered negative, wrote the group led by Dr. Sebastian Bickelhaupt from the German Cancer Research Center in Heidelberg (Radiology, September 29, 2015).
Abbreviated protocols
While adding MRI as an adjunct to conventional mammography could help reduce the latter's high false-positive rate, the disadvantage is that MRI exams can be time-consuming and often require contrast.
However, recent papers have extolled the benefits of abbreviated breast MRI protocols, the authors noted. As a result, they chose to investigate a protocol consisting of maximum intensity projections (MIPs) from DWIBS and unenhanced morphological sequences. Their goal was to compare this unenhanced protocol with an abbreviated contrast-enhanced protocol and also full diagnostic breast MRI.
The prospective study enrolled 50 women at two imaging sites between September 2014 and January 2015. The subjects had a mean age of 57.1 years (range, 50-69 years), suspicious screening mammogram results, and an indication for biopsy. MRI exams were performed on a 1.5-tesla scanner (Ingenia, Philips Healthcare) with a dedicated seven-channel breast coil.
The two readers were blinded to each other's interpretations and to all clinical data, screening mammography studies, and screening reports. They were aware, however, that subjects may have a suspicious lesion from their screening x-ray mammograms because that information was part of the study's inclusion criteria.
MR images were rated on a five-point scale, with 1 indicating that no suspicious lesion was detected and 5 indicating a highly suspicious lesion with biopsy recommended.
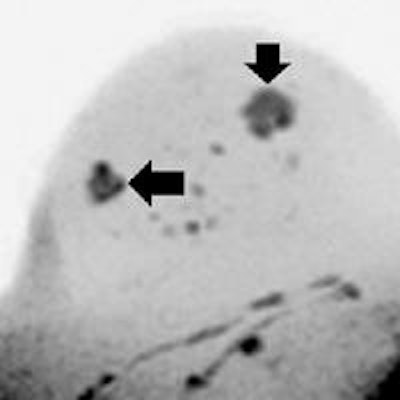
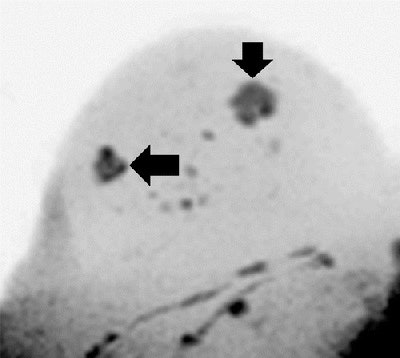 Images are of a 51-year-old woman. DWIBS MIP (above), displayed with black-white inversion, shows one lesion seen at screening (horizontal arrow) and a second lesion seen with the DWIBS protocol (vertical arrow). Transverse T2-weighted turbo spin-echo MR image (below) allows clarification of the second lesion as a simple cyst. Histopathologic examination revealed an invasive ductal carcinoma in the solid lesion, while the water-intense second lesion was an uncomplicated cyst. Images courtesy of Radiology.
Images are of a 51-year-old woman. DWIBS MIP (above), displayed with black-white inversion, shows one lesion seen at screening (horizontal arrow) and a second lesion seen with the DWIBS protocol (vertical arrow). Transverse T2-weighted turbo spin-echo MR image (below) allows clarification of the second lesion as a simple cyst. Histopathologic examination revealed an invasive ductal carcinoma in the solid lesion, while the water-intense second lesion was an uncomplicated cyst. Images courtesy of Radiology.Lesion detection
Of the 50 patients, 24 (48%) had a malignant lesion. Twenty-one women (88%) had invasive ductal carcinoma, two (8%) had ductal carcinoma in situ (DCIS) as the only finding, and one (4%) had invasive lobular carcinoma. Benign lesions were found in 26 participants (52%), including seven cases (27%) of fibrosis or metaplasia and four cases (15%) of fibrocystic metaplasia.
With both abbreviated protocols, the readers missed the two DCIS lesions due to clustered microcalcifications. With the contrast protocol, the second reader also missed two invasive cancer lesions, while the first reader missed one such lesion.
The DWIBS approach was positive in 100% of the histopathologically confirmed invasive breast cancers in the screening population, excluding the two lesions with pure microcalcifications, which the authors described as "notoriously invisible" on MRI.
In addition, there was no statistically significant difference between the accuracy of the full diagnostic protocol and the accuracies of the abbreviated protocols, the group noted.
| Abbreviated and full protocols for breast MRI | ||||
| Sensitivity | Specificity | Negative predictive value | Positive predictive value | |
| DWIBS protocol | 92%* | 94%* | 92% | 93% |
| Contrast protocol | 85% | 90% | 87% | 89% |
| Full diagnostic MRI protocol | 92% | 92% | 92% | 92% |
| Screening mammography | 75% | 94% | 99% | 92% |
The mean image acquisition time was less than seven minutes for the DWIBS protocol and less than five minutes for the abbreviated contrast protocol, not taking into account IV preparation and contrast device testing. This compares with more than 30 minutes for a full breast MRI protocol, according to the authors.
In cases with no suspicious findings, mean reading time was 2.82 ± 1.26 seconds for the DWIBS protocol and 4.05 ± 2.67 seconds for the contrast protocol. When there were suspicious findings, overall reading time was 29.8 ± 16.7 seconds for DWIBS and 29.8 ± 16.1 seconds for the contrast protocol.
In 11 (42%) of the 26 benign cases, the findings could be diagnosed by reading the DWIBS MIPs only, with a reading time of less than three seconds for those participants.
The researchers cited several limitations of the study, including its preselected patient group, which had a greater probability of malignant lesions than the regular population. Therefore, they did not form any conclusions about the efficacy of DWIBS to screen an "unselected population."
In conclusion, Bickelhaupt and colleagues described their DWIBS mammography protocol as "highly accurate in ruling out malignancy" detected on x-ray screening mammograms "if it is used as a complement after the screening clarification procedure."