LOS ANGELES - Can MR be used safely in patients like combat veterans, who often have retained metal fragments in their bodies? Yes, but proceed with caution, according to research presented at the American Roentgen Ray Society (ARRS) meeting.
Combat veterans often have retained metal fragments that can range from bullets or bullet fragments to pellets, BBs, or shrapnel -- items that can cause artifacts on MRI scans, or even move inside the patient's body due to the scanner's powerful magnetic field.
When these patients need diagnostic imaging -- and when MR would seem to be the best exam -- radiologists should carefully consider a number of factors before sending them to the MR suite, said presenter Dr. Dane Van Tassel of the Maricopa Integrated Health System in Phoenix.
"A 1.5-tesla magnet is more than 30,000 times more powerful than the Earth's magnetic field," he said. "An MR can pull forklift tines off machines and turn stretchers and mop buckets into projectiles. So identifying metal foreign objects before a patient who is a veteran undergoes MR is especially important."
Finding fragments
The problem is that veterans still need access to MR, according to Van Tassel.
"Receiving MR can put patients in this population at increased risk for adverse events," he said. "But denying them the exam limits the evaluation of pathologies for which MR is best."
Prior in vivo studies have used data from criminal trauma cases to evaluate how metal fragments behave in MR. They found that bullets containing steel or ferromagnetic compounds can heat up, migrate, or rotate in the MR device. This research is a good start, but there's still the need for evidence-based guidelines on how to safely use MR in patients with retained metallic fragments sustained during warfare, Van Tassel told session attendees.
"In contrast to something like a pacemaker, we don't know the mechanism or the composition of these foreign bodies, and that's why they've been traditionally considered unsafe," he said.
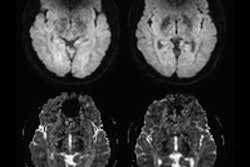
For their research, Van Tassel and colleagues conducted a retrospective analysis of 8,298 patients with metal fragments who underwent MRI exams between February 2014 and March 2015 at the Veterans Affairs Medical Center in Phoenix. The team reviewed x-rays of the parts of the patients' bodies with the retained metal, analyzing where the fragments were and how close they were to vital structures such as large vessels or nerves, organs, or the spinal canal.
Of the total cohort, 76 had known or suspected metal fragments in their bodies. The majority of these fragments were in the patients' extremities, both upper and lower.
Three radiologists discussed each case and came to a consensus about whether an MR exam would be safe. They used the following criteria:
- Is the fragment centrally or peripherally located?
- Is its proximity to a vital structure greater than 1 cm?
- How many fragments are there? How big is the largest one?
- How are the fragments shaped? Are they smooth or jagged?
- Has the patient had any previous MR exams without incident?
- What is the risk-benefit ratio? Is an MR exam clinically warranted? Would another study be safer?
Of the 76 patients who had metal fragments in their bodies, 62 (82%) were cleared for MR imaging, according to Van Tassel. Most of the fragments were in patients' extremities.
"All 62 patients completed the MR exam without adverse incident," he said.
Proceed, but with caution
Van Tassel and colleagues undertook this study as validation research for a prospective study they plan to conduct soon. In the meantime, he urged radiologists to err on the side of caution when it comes to MRI and veterans.
"Use abundant caution in interpreting and applying our findings," he told session attendees. "Our study was limited by the fact that it was a retrospective evaluation and had a small sample. The safety of our approach needs to be systematically evaluated with a prospective study."