Abnormalities detected on MRI scans of knee cartilage can be a reliable predictor of future defects due to osteoarthritis and could signal the risk of cartilage degeneration, according to a study published online May 2 in Radiology.
The group from the University of California, San Francisco (UCSF) also found a significant link between baseline MRI signal abnormalities, subsequent cartilage regression, and the presence of bone marrow abnormalities.
"These results suggest that cartilage signal abnormalities represent early abnormal changes in the cartilage, which eventually may develop into morphologic defects," wrote lead author Dr. Benedikt Schwaiger and colleagues from UCSF's departments of radiology and biomedical imaging and epidemiology and biostatistics (Radiology, May 2, 2016).
Damage assessment
Osteoarthritis is the most prevalent chronic joint disease in the U.S., due primarily to an aging population and an increase in the number of obese people. MRI has played a key role in early diagnosis, which could lessen the condition's effects later in life. While tools have been developed to help assess a person's degree of osteoarthritis, previous studies have been inconsistent in determining the value of signal abnormalities found on baseline MRI scans of cartilage and their potential link to future joint degradation, the authors noted.
"To our knowledge, the evolution of signal abnormalities has never been analyzed longitudinally, and the progression rate and effect of signal abnormalities on joint degeneration is unclear," Schwaiger and colleagues wrote.
The researchers used data from 90 subjects with and without risk factors for knee osteoarthritis who were enrolled in UCSF's Osteoarthritis Initiative. The ongoing longitudinal, prospective, multicenter study is sponsored by the U.S. National Institutes of Health and is designed to explore the diagnosis, treatment, and prevention of osteoarthritis.
Participants had a mean age of 54 years (± 5 years) and had no cartilage signal abnormality or morphologic defect when baseline MRI scans were acquired. MRI scans were conducted on identical 3-tesla scanners (Trio, Siemens Healthineers) at all four participating imaging centers.
The MR imaging protocol included a sagittal intermediate-weighted fat-saturated 2D fast spin-echo sequence to determine the presence and signal characteristics of cartilage signal abnormalities. A coronal 2D fast spin-echo sequence and a sagittal T2-weighted 3D dual-echo steady-state sequence were used to determine any morphologic cartilage changes and to evaluate knee joint structures.
The MRI scans were repeated after 48 months. At that time, radiologists could view the baseline and follow-up images side by side to evaluate cartilage changes and signal abnormalities.
Signal connections
The baseline MRI scans revealed cartilage signal abnormalities in 126 individual areas, or compartments, with no compartment showing more than one signal abnormality.
Of the 90 subjects, 22 (24%) had signal abnormalities in two compartments, four (5%) showed signal abnormalities in three compartments, and two (2.5%) had signal abnormalities in four compartments.
Among the 126 individual cartilage MRI signal abnormalities, 72 (57%) showed a morphologic cartilage defect at the 48-month mark. In comparison, only 4% of compartments without signal abnormalities showed morphological defects.
Perhaps most importantly, cartilage signal abnormalities were associated with bone marrow abnormalities in 37 (29%) of the 126 abnormal compartments. Conversely, bone marrow abnormalities were discovered in only eight (1.5%) of the 540 compartments with no baseline signal abnormalities.
"We found no further parameters besides the association with bone marrow abnormalities that would enable us to predict the development of a morphologic defect in a patient with a pre-existing signal abnormality," the authors wrote.
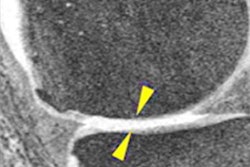
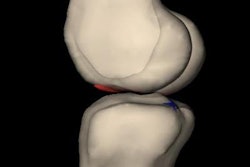
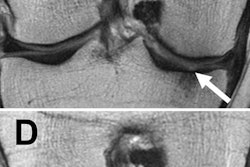
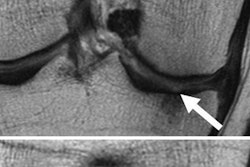
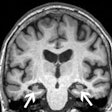
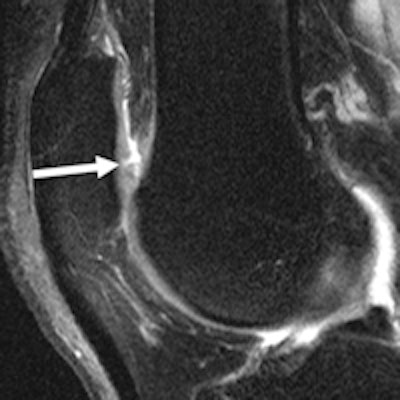
 MR images of the right knee show signal abnormalities at baseline and subsequent defects at the 48-month follow-up. Above image shows a hyperintense signal abnormality in the patella at baseline (arrow). Image below shows the development of a fissure in the same patient (arrow) at 48 months. Images courtesy of Radiology.
MR images of the right knee show signal abnormalities at baseline and subsequent defects at the 48-month follow-up. Above image shows a hyperintense signal abnormality in the patella at baseline (arrow). Image below shows the development of a fissure in the same patient (arrow) at 48 months. Images courtesy of Radiology.In an analysis by compartment, data revealed that cartilage signal abnormalities were most frequent in the patella (44 cases, 35%), followed by the lateral tibia (33 cases, 26%), trochlea (31 cases, 25%), medial femur condyle (10 cases, 8%), lateral femur condyle (7 cases, 6%), and medial tibia (1 case, 1%).
Given the association between baseline cartilage MRI signal abnormalities and subsequent degenerative changes in musculoskeletal joints, the findings "suggest that cartilage signal abnormalities represent early abnormal changes in the cartilage, which eventually may develop into morphologic defects," Schwaiger and colleagues wrote.
In addition, a "promising next step might be to assess compositional imaging parameters, such as T1 and T2 imaging, in signal abnormalities," since both techniques "have been identified as valid biomarkers for early cartilage degeneration" in previous studies.
"Therefore, they may enable us to predict the development of a morphologic defect in cartilage in patients with a pre-existing signal abnormality," they wrote.