Performing breast MRI in the supine position in the operating room (OR) immediately after breast conservation surgery may help surgeons better find and assess residual tumors, while patients potentially avoid follow-up surgery, according to a new study published online June 22 in Radiology.
In a new phase I clinical trial, clinicians at Brigham and Women's Hospital (BWH) in Boston found significant differences and additional information on breast deformity and tumor position in intraoperative supine MR images, which ideally would lead to more effective cancer removal, compared to images from a more conventional preoperative prone MRI scan.
"We did the supine MRI at the time of the surgery to show the tumor to the surgeon; and after surgery, we did an additional supine MRI to see if there were any more tumors," explained lead author Dr. Eva Gombos, a BWH radiologist. "Then surgeons could do an incision on the spot [if needed], so the patient did not have to return for another operation."
Breast conservation
One way to plot the most appropriate course of action for breast cancer is to determine if the patient has a positive margin, in which cancer cells appear on the edges of removed tissue and indicate a higher risk of recurrence. A clear margin indicates there are no cancer cells on the edges of removed tissue and the patient is a candidate for breast conservation therapy.
"However, the problem with breast surgery is that the margins for surgery are not that clear in as many as 40% of cases in the U.S.," Gombos told AuntMinnie.com.
 Dr. Eva Gombos from Brigham and Women's Hospital.
Dr. Eva Gombos from Brigham and Women's Hospital.Traditionally, patients who are scheduled to undergo breast conservation surgery, or lumpectomy, are placed in a prone position, face down, with the breast fitted with an MRI coil and hanging through a hole. The prone MRI position does have better image resolution, primarily because clinicians use a breast coil to enhance visualization.
Previous studies, however, have questioned whether preoperative MRI for surgical planning or to evaluate breast cancer leads to improved surgical outcomes, the authors noted.
The dilemma is that preoperative MR images are taken from a prone position, but the patient is in the supine position (face up, on her back) for surgery with gravity naturally changing the shape of the breast.
Between April 2012 and November 2014, 12 patients underwent standard diagnostic MRI in the prone position as an outpatient prior to surgery. Six of those women also had supine MRI scans before their operation (Radiology, June 22, 2016).
The MRI-guided breast conservation surgery was performed in a multimodality operating suite, which featured a ceiling-mounted, 70-cm bore, 3-tesla MRI scanner (Verio, Siemens Healthineers) in the center of the room that could be moved in and out of the surgical field.
All MR images and information relevant to the procedure were accessible in the operating suite, allowing radiologists and surgeons to continuously view imaging data.
Tumor changes
In reviewing images from the preoperative prone MR with images from the intraoperative supine MR, the researchers found tumor displacement in the six patients who had both prone and supine MRI scans. The average tumor displacement was 23.8 mm in the lateral coordinate, -27.7 mm in the anterior coordinate, and -6.5 mm in the superior coordinate. As expected, tumors were closer to the chest wall on supine images than on prone images.
There were also noticeable changes in tumor formation, such as volume, surface area, and sphericity, with the different patient positions.
| Mean differences in tumor deformation, prone vs. supine imaging | |
| Volume | 23.8% |
| Surface area | 6.5% |
| Compactness | 16.2% |
| Sphericity | 6.8% |
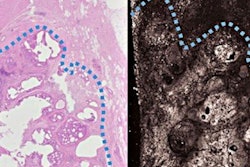
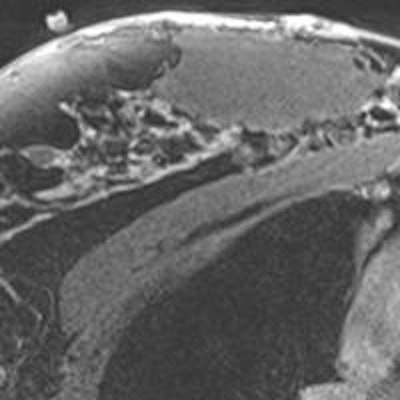
 MR images are from a 43-year-old patient who underwent lumpectomy in the OR imaging suite for a 2-cm right upper inner quadrant invasive mixed ductal and lobular cancer. The prone MRI (above) is a postcontrast axial T1-weighted fat-suppressed MR sequence that shows rapid enhancement of the tumor. The postprocedural supine unenhanced axial T1-weighted fat-suppressed MRI (below) taken in the OR imaging suite shows the tumor cavity and the skin markers. Images courtesy of Radiology.
MR images are from a 43-year-old patient who underwent lumpectomy in the OR imaging suite for a 2-cm right upper inner quadrant invasive mixed ductal and lobular cancer. The prone MRI (above) is a postcontrast axial T1-weighted fat-suppressed MR sequence that shows rapid enhancement of the tumor. The postprocedural supine unenhanced axial T1-weighted fat-suppressed MRI (below) taken in the OR imaging suite shows the tumor cavity and the skin markers. Images courtesy of Radiology.The good news is that all patients underwent successful removal of their tumor with clear margins for invasive breast cancer.
In addition, the mean duration time of the preoperative supine MRI scan was 25 minutes (range: 17.7-37 minutes), while the postoperative supine MRI had a mean time of 19 minutes (range: 15.1-22.9 minutes).
Clinical implications
Given the considerable changes in breast deformity and tumor locations closer to the chest wall, Gombos and colleagues suggested that supine MRI before surgery may provide surgeons with more detailed and accurate information and could lead to more effective tumor removal.
"We were not first to demonstrate that everything is closer to the chest wall in the supine position; there were other studies," Gombos added. "But we combined the supine MRI on the spot in the operating room, which makes the tumor location more exact for surgery to be done in the supine position."
The BWH researchers plan to expand their current study and further reduce the need for reoperation, which negatively impacts the patient emotionally, delays postoperative therapy, and increases infection rates and cost.
"I am not advocating not using prone MRI, if it is the way to get the best image resolution," Gombos said. "However, we added the supine MRI with the goal of having the clearest margins and helping the patients."
One focus of the future research will be to avoid the extra time in the surgical suite for the postoperative supine MRI.
"A full MRI study in the OR would add 20 to 30 minutes," Gombos said. "It is too long for the patient to be in the OR for that extra time under anesthesia. It is not what we recommend."