The desire to avoid exposing pediatric patients to CT's ionizing radiation appears to be powering increased use of MRI at one New York City hospital's emergency department (ED). The shift to the modality is also prompting the facility to adjust resources to meet times of greatest volume and demand.
Pediatric patients who visit the ED at Children's Hospital at Montefiore in the Bronx are most likely to undergo MRI scans in the evening and during the middle of the week. A great majority of procedures are performed for neurological reasons, such as a headache, seizure, trauma, or weakness, according to a study presented at RSNA 2016 in Chicago.
"Possible causes of this increased MRI utilization are the desire to decrease the use ionizing radiation. This is collaborated by our finding of a decrease in CT usage," said lead author Dr. Miriam Hulkower, a radiology resident at Montefiore Medical Center. "Our long-term goal is to modify radiologists and scanner availability so that studies may be performed and read in a timely manner."
MRI's advantages
The benefits of MRI for pediatric imaging certainly are well-accepted. The modality contributes to the goal of avoiding ionizing radiation, which has become an increasingly sensitive issue in this patient population. MRI also has the ability in certain clinical applications to detect additional pathologies that may not be seen on CT.
 Dr. Miriam Hulkower from Montefiore Medical Center.
Dr. Miriam Hulkower from Montefiore Medical Center."However, there are some challenges in using MRI in the emergency room, including 24/7 availability in only some hospitals, radiologists may not be available to read the studies 24/7, MRI has a longer imaging time, and, therefore, [there is] a longer wait time to perform the studies," Hulkower said.
To further investigate these factors and how they influence pediatric patient care, the researchers retrospectively reviewed records from all MRI and CT scans performed from 2011 to 2015 at the Children's Hospital at Montefiore. Two MRI scanners were available from 8 a.m. to 12 midnight, while one scanner was available from midnight to 8 a.m.
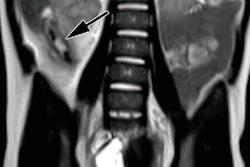
To further determine utilization, the researchers divided MRI and CT scans into three categories: neurological, which included brain, head and neck, MR angiography, and spine; trunk imaging, which included the chest, abdomen, and/or pelvis; and musculoskeletal.
Numbers crunch
During the five-year study period, the hospital's emergency department had 280,845 pediatric visits, with 997 MRI scans performed on 776 patients (1.3 scans per patient) for a utilization rate of 0.28%. Over the course of the study, the researchers found a statistically significant increase in utilization, with MRI performed during 0.12% of visits in 2011 and 0.24% of visits during 2015.
| Reasons for pediatric MRI scans from 2011 to 2015 | ||
| Brain | 57% | |
| Spine | 15% | |
| Neurologic MR angiography | 13% | |
| Abdomen | 6% | |
| Face | 5% | |
| Musculoskeletal | 4% | |
The advance in MRI usage was driven primarily by neurological imaging, which increased from a utilization rate of 0.23% in 2011 to 0.49% in 2015. The rate of musculoskeletal MRI scans stayed steady throughout the five years.
"Trunk exams overall stayed steady until the final year of the study (2015) when there was an uptick, likely due to an emphasis on performing more MRIs than CTs for appendicitis workups," Hulkower told RSNA attendees.
By comparison, overall CT utilization decreased from a rate of approximately 1.75% in 2011 to approximately 1.55% in 2015. The decline in CT utilization in the ED mirrored the drop in neurological CT scans, which slipped from a rate of 1.4% in 2011 to approximately 1.15% in 2015. Trunk and musculoskeletal CT scans remained relatively steady during the five-year period.
Gender differences
Interestingly, more female pediatric patients underwent neurological MRI scans than their male counterparts, with a ratio of 1.4 to 1. One possible explanation is that girls presented with a higher rate of headaches. The researchers also found that ED clinicians used fast spine T2 imaging sequences to rule out hydrocephalus.
Young female patents also received 4.3 times as many trunk MRI scans than male patients. Hulkower and colleagues credited a higher suspicion of appendicitis, which mimics adnexal pathology possibly related to the ovaries, fallopian tubes, or uterus.
On the other hand, pediatric male patients were twice as likely (2.1 to 1) to undergo musculoskeletal scans, compared with female patients, because of a higher rate of sports-related injuries and bone tumors among males.
MRI utilization was also associated with age. The frequency of MRI scans for pediatric patients 5 years and younger was 0.1% or less, because ED staff preferred to avoid sedation for the youngest patients. The rate of MRI scans rose to 0.35% for 6-year-old children and peaked at slightly more than 1% at age 17.
As for when MRI scans were performed, traffic peaked between 7 p.m. and 10 p.m., while Tuesdays, Wednesdays, and Thursdays experienced the highest volume. Increased utilization during the evening and nighttime hours and minimal usage during morning hours had important clinical implications at the Children's Hospital.
"As we recruit ED physicians, our overnight division has focused on finding multispecialty radiologists with neuroradiology training to read these studies," Hulkower said. "In addition, the division head of pediatric radiology has lectured and brought in grand-rounds speakers on the interpretation of emergency abdominopelvic MRI scans."
Utilization forces
Based on the results, Hulkower and colleagues concurred that the increase in MRI utilization was due, in part, to the desire to avoid ionizing radiation exposure to the pediatric patients.
"This is collaborated by our finding of a decrease in CT usage," Hulkower added. "In addition, there is a physician desire to make a definitive diagnosis or rule out a specific diagnosis while in the ED, possibly to avoid a costly hospital admission or to avoid medical-legal concerns."
The researchers cited a few limitations of the study, including the fact that it was conducted at a single institution.
"However, our findings may be applicable to other large, urban academic centers," Hulkower said. "A follow-up study will be needed to conform this. Other centers can perform a similar analysis in their own institution in order to focus their pediatric MRI resource needs."
Also, the researchers did not perform an assessment on the appropriateness of each MRI scan, nor did they consider drawbacks of MRI in the ED, such as the increased cost of the exam or a potentially longer stay in the ED.