Given the ongoing concern over the safety of gadolinium-based contrast agents (GBCAs), researchers have developed a resource for MRI technologists and radiologists that calculates accurate and appropriate GBCA doses for patients to avoid dosing errors.
The Gadolinium Dose Calculator provides access to package inserts for all GBCA products approved by the U.S. Food and Drug Administration (FDA). The calculator is available online and for smartphones, and it was created at the University of Wisconsin (UW) and University of California, Santa Cruz. The main goal of the calculator is to ensure patient safety during all MRI scans.
"Since we have been using the gadolinium calculator, we have not had any incidents with misdosing," said lead researcher Dr. Scott Reeder, PhD, chief of MRI at the University of Wisconsin. "Those [incidents] were extremely uncommon anyhow, but we generally feel more confident that we are providing a safe environment by having this available for our technologists."
Gadolinium formulas
Reeder, who also serves as director of UW's liver imaging research program, presented details of the Gadolinium Dose Calculator last month at the International Society for Magnetic Resonance in Medicine (ISMRM) annual meeting.
 Dr. Scott Reeder, PhD, from the University of Wisconsin.
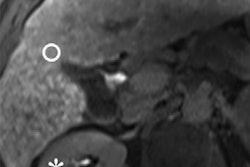
Dr. Scott Reeder, PhD, from the University of Wisconsin.Gadolinium-based contrast agents were introduced to MR imaging in 1987. The first five GBCAs approved for clinical use by the FDA had the same formulation of 0.5 M and approved dose of 0.1 mmol/kg.
This uniformity led to the unfortunate and widespread use of terminology such as "single dose" and "double dose," Reeder wrote in a 2014 article (Journal of Magnetic Resonance Imaging, June 2014, Vol. 39:6, pp. 1343-1345). The introduction of gadoxetic acid (0.25 M, 0.025 mmol/kg), gadofosveset trisodium (0.25 M, 0.03 mmol/kg), and gadobutrol (1.0 M, 0.1 mmol/kg) added different formulations and approved doses, creating opportunities for dosing errors and confusion.
Even with the differences between the gadolinium products, MRI technologists and radiologists are taught early in their careers to figure out the correct GBCA volume by multiplying the recommended dose (mmol/kg) by weight (kg) and dividing that number by concentration (mmol/mL).
"All technologists and radiologists who use MRI on a regular basis should understand that [equation], but to do the calculation when you are in a hurry is more challenging from a practical perspective than you would think," Reeder told AuntMinnie.com.
In a busy environment, technologists may not have the time or inclination to use the formula. At those times, they might turn to a GBCA dose table for guidance.
"The problem with tables is when you come across a patient with an unusual weight -- either big or small -- or the radiologist has to use a nonstandard dose, then they do not have the correct number," Reeder said. "So there was a real need to develop an easy-to-use method for calculating an accurate gadolinium dose on the fly."
The Gadolinium Dose Calculator features safeguards: If a technologist or radiologist enters the wrong dose or if the number exceeds the recommended maximum dose based on a patient's weight, then a pop-up window will alert the user to the error.
There also are links to each GBCA's package insert, which can be viewed immediately on a workstation or smartphone or downloaded and stored for future offline access.
Off and running
The Gadolinium Dose Calculator app (GadCalc) is currently available through iTunes. Since its release in November 2015, there have been 239 unique installations from five countries, including 55% from within the U.S.
For the online calculator, Google Analytics has shown 22,074 page visits and 9,841 unique views since February 1, 2016. While the majority of unique page visits have come from the U.S. (93%), the calculator has also been accessed from 68 different countries.
Closer to home, workstations with internet connectivity are located next to all MRI scanners at all UW inpatient and outpatient sites for immediate access to the calculator. In addition, members of UW's MRI research program and many outreach locations served by the university have come to rely on the gadolinium guidance.
"The feedback has been primarily from our own technologists," Reeder said. "There was one day when a web server was down and [UW technologists] were immediately knocking on my door asking, 'Where is the gadolinium calculator? It's not working today.' That was positive feedback that they use it and they need it."
The researchers' next project is to make the technology accessible on the Android platform and enhance the app's usability. Another continuing goal is to keep the service free of charge for users.
"There are some small charges that Apple charges us to have the app in the iTunes Store, but we feel it is in our best interests and to take care of our own patients to cover [the charges]," Reeder added. "It has been a fun project. We are very pleased to see how much traction it has gained both internally and externally."