European researchers have developed a functional liver imaging score (FLIS) that uses gadoxetic acid-enhanced MRI to help predict which patients with advanced chronic liver disease might need a transplant or are at greater risk of mortality, according to a study published online November 19 in Radiology.
The FLIS approach combines three hepatobiliary-phase features obtained 20 minutes after injection of gadoxetic acid. Each component is rated on a scale of 0 to 2. The higher the scores, the greater the likelihood that the patient will have a longer transplant-free survival.
"Because the FLIS requires no signal intensity measurements, equations, or specific software, and is independent of MRI field strength and vendor, it has the potential to be implemented easily in routine clinical practice," wrote the authors, led by Dr. Nina Bastati from the Medical University of Vienna.
The functional liver imaging score technique was introduced in a 2016 study in which Bastati et al validated its efficacy in a review of 128 patients who had undergone liver transplants. The FLIS approach proved "superior" to a number of clinical and laboratory parameters that are known for reliably predicting graft survival for these patients.
The FLIS combines the three following components:
- An enhancement quality score based on whether the liver is hypointense, isointense, or hyperintense, relative to the right kidney
- An excretion quality score, which indicates the degree of contrast agent excretion into the biliary tract
- A portal vein sign quality score based on whether the portal vein is hyperintensive, isointensive, or hypointense compared with the liver parenchyma
As the sum of all three parameters, which are equally influential in determining the condition of a patient with chronic liver disease and their chance for survival, the FLIS ranges from 0 to 6 points. For the current study, the researchers hypothesized that "patients with a low FLIS are at higher risk for the development of hepatic decompensation and mortality compared with patients with a high FLIS."
To that end, the team analyzed 265 patients (mean age, 53 ± 14 years) who underwent 3-tesla MRI scans (Magnetom Trio, Siemens Healthineers) with a standard dose (0.025 mmol/kg) of gadoxetic acid (Primovist/Eovist, Bayer HealthCare Pharmaceuticals) followed by a 20-mL saline flush. Patients were divided into three groups based on fibrosis stage:
- Nonadvanced chronic liver disease
- Compensated advanced chronic liver disease in which the liver is damaged by cirrhosis but can still function
- Decompensated advanced chronic liver disease, which is caused by hepatitis or excessive alcohol intake
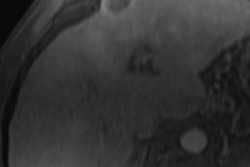
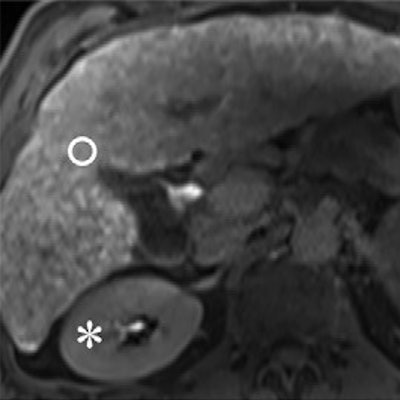
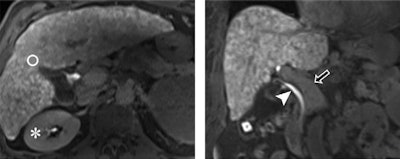 Images from 3-tesla MRI acquired 20 minutes after gadoxetic acid administration in a 61-year-old man with alcohol-induced cirrhosis and a FLIS of 6. His liver parenchymal enhancement quality score was 2, due to higher signal intensity of the liver (circle) compared with the right kidney (*). Excretion quality score is 2 from contrast media in the common bile duct (arrowhead). Portal vein sign quality score was 2 because the portal vein (arrow) was hypointense to the liver parenchyma. Images courtesy of Radiology.
Images from 3-tesla MRI acquired 20 minutes after gadoxetic acid administration in a 61-year-old man with alcohol-induced cirrhosis and a FLIS of 6. His liver parenchymal enhancement quality score was 2, due to higher signal intensity of the liver (circle) compared with the right kidney (*). Excretion quality score is 2 from contrast media in the common bile duct (arrowhead). Portal vein sign quality score was 2 because the portal vein (arrow) was hypointense to the liver parenchyma. Images courtesy of Radiology.Using an optimal FLIS cutoff of 4, the researchers achieved two goals. They accurately predicted 12-month transplant-free survival in 87 (92%) patients with compensated advanced chronic liver disease and were correct in survival prediction for 37 (71%) patients with decompensated advanced chronic liver disease.
Overall, nine patients (8%) in the compensated advanced chronic liver disease underwent liver transplant and 24 patients (22%) died. Among the decompensated advanced chronic liver disease patients, 19 people (19%) underwent a liver transplant and 48 patients (49%) died.
"Our study demonstrates that the FLIS is an independent predictor of liver-related events and transplant-free survival in patients with different causes of chronic liver disease," the researchers concluded. "Both decompensated and compensated patients with chronic liver disease, with a reduced FLIS showed a three- to sevenfold higher risk of mortality, even after adjusting for established prognostic factors."