Could performing MRI scans on individuals who present to the emergency department (ED) with symptoms of multiple sclerosis (MS) cut how long they end up staying in the hospital? Researchers from Johns Hopkins reported interesting findings in a new study.
The group found that performing MRI scans on patients with MS symptoms cut as much as half a day from their length of stay as hospital inpatients, without significantly adding to the amount of time they spent in the ED. While the calculations fell slightly short of statistical significance, the results could support efforts for earlier discharge of MS patients, which in turn could help reduce hospital overcrowding, save money for patients, and improve patient flow through the ED.
"One benefit is that you could reduce the length of stay in the hospital, and another major benefit would be to avoid the needless hospital admission," said lead author and research fellow Dr. Jina Pakpoor.
MRI in the ED
Johns Hopkins installed an MRI scanner in its tertiary facility's emergency department in 2012. Part of the reason was for stroke treatment certification, which requires 24-hour access to MR imaging. However, ED staff soon found that the modality was also beneficial for evaluating other neurological conditions, such as multiple sclerosis.
 Dr. Jina Pakpoor from Johns Hopkins.
Dr. Jina Pakpoor from Johns Hopkins.An MS exacerbation is a "flare-up of symptoms that is reflective of underlying inflammation or disease progression, which is what sets [MS] apart from a more common alternative diagnosis," Pakpoor explained to AuntMinnie.com.
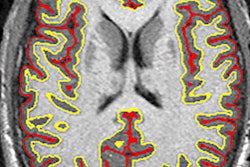
To evaluate the symptoms, clinicians generally turn to diffusion-weighted MR imaging (DWI-MRI) to determine demyelination, which is the erosion of the myelin sheath that protects nerve fibers and nerve impulses.
Pakpoor and colleagues hypothesized that when MS patients with exacerbations underwent an MRI scan in the ED, their length of stay in the ED would naturally increase. Conversely, if they were admitted to the hospital, given the information gained with the ED MR images, their inpatient length of stay would decrease.
The researchers reviewed ED admissions of all patients with a previously known MS diagnosis who were treated for MS exacerbations, and who were admitted as hospital inpatients from the ED between May 2013 and May 2016.
Admission factors
A total of 81 patients met the study's inclusion criteria, with 56 MS patients (69%) undergoing MRI scans in the ED. The other 25 patients (31%) did not have an emergency MRI scan, but they were admitted to the hospital where they were imaged as inpatients.
"We looked at the radiology reports that utilize the emergency department MRI scanner. Then we looked at a separate set of data that the neurologist had for that patient that utilized the inpatient scanner," added Pakpoor, who presented the study results earlier this month at the American Roentgen Ray Society (ARRS) annual meeting.
| Effect of MRI scans on MS patient length of stay | ||||
| MS patients without ED MRI | MS patients with ED MRI | Difference | p-value | |
| Department length of stay | 7.5 hours | 8.1 hours | 36 minutes | 0.456 |
| Admission length of stay | 3.1 days | 2.6 days | 13.3 hours | 0.1010 |
The 13-hour difference in admission length of stay tacked on an additional day's hospital fee for discharges between midnight and 1 p.m. for five patients, the researchers noted. In addition, MRI scans on four MS inpatients showed their symptoms were pseudoexacerbations, which prompted the question of whether their mean inpatient length of stay of 3.1 days was unnecessary.
While the results did not reach statistical significance, a 13-hour reduction in hospital length of stay could have clinical implications for early discharge, Pakpoor said.
"Thirteen hours can make the difference between arranging for an earlier day's discharge or early-in-day discharge," she said. "I think more broadly the utility of ED imaging is as much for avoiding needless management and ruling out urgent sinister conditions as it is for reducing the length of stay."
In fact, Johns Hopkins in 2013 began implementing measures to discharge MS patients who are admitted for exacerbations as early in the day as possible to avoid additional charges. The emergency department MRI scanner has become an integral tool in that strategy.
"The potential downside with the ED MRI scanner is that we don't want a situation where emergency department physicians rely more heavily on the MRI scanner to accept a diagnosis, just because [the MRI] is available," Pakpoor added.
The findings have not prompted any major protocol changes in terms of how Johns Hopkins' ED clinicians approach MS exacerbations, but the researchers do plan to expand their study on the use and potential benefits of the ED MRI scanner.
"I would hope that an increasing number of institutions introducing an MRI scanner into their emergency departments would further investigate the impact that the radiologist can have in that early stage [of diagnosis] and making those important management decisions as early as possible," she said.
Other potential benefits would be the reduction of overcrowding in the ED, which previous literature has described as a "national epidemic," Pakpoor said. The availability of an MRI scanner in the ED may also reduce imaging wait times for hospital inpatients.