Using MRI on women with breast cancer within one year of their giving birth can achieve sensitivity of almost 100% for detecting tumors and change surgical management in more than one in four cases, according to a study published in the September issue of the American Journal of Roentgenology.
The findings contradict the common view that pregnancy-related hormonal changes and background parenchymal enhancement make breast MRI ineffective for women with pregnancy-associated breast cancer (AJR, September 2017, Vol. 209:3, pp. W177-W183).
"The bottom line is that we should not be dissuaded from using preoperative breast MRI just because a patient is in the first year of postpartum," said lead author Dr. Kelly Myers, an assistant professor of radiology at Johns Hopkins Medical Institutions. "Before our study, we might have hesitated whether or not to use MRI for these patients, because we read that [MRI's] utility may be limited. Now that we have this data, we can show that MRI is helpful in that first year of postpartum."
Unique circumstances
Pregnancy-associated breast cancer is defined as breast cancer that occurs in the first year postpartum. It's quite rare, occurring only once in 3,000 to 10,000 pregnancies, according to some estimates. However, when the disease does manifest, it is often aggressive and is associated with a greater rate of recurrence and death, compared with other age- and stage-matched cancers.
"There is a theory that it could be the hormones of the pregnancy in a postpartum state that fuel the tumors," Myers told AuntMinnie.com. "That is possible, but that is still up for debate."
Also lacking are studies that target this patient population. Myers and colleagues found only one paper on the use of breast MRI among postpartum women, and that study only covered a handful of subjects.
"The largest study published to date looking at this patient population with MRI had only five patients," she said. "It seemed like a big void in research that we could fill."
For their study, the researchers retrospectively reviewed medical records ranging from January 1994 to May 2014, identifying 53 women at Memorial Sloan-Kettering Cancer Center who met the study's criteria. The subjects had a mean age of 36 years (± 3.5 years; range, 29-43 years) when they were diagnosed with breast cancer either during their pregnancy or within one year of delivery.
Nine patients were pregnant at the time of their cancer diagnosis but were not scanned until after giving birth and before receiving treatment. The other 44 women (83%) presented with cancer during their first year postpartum.
"We do not perform MRI scans on anyone who is pregnant," Myers added. "While the study included patients with pregnancy-associated breast cancer, it was defined as breast cancer diagnosed during pregnancy or the year following delivery. So all 53 patients who had MRI scans in the study were postpartum and were not pregnant at the time of the MRI."
The majority of women (45, 85%) presented with palpable abnormalities; 52 patients (98%) were diagnosed with invasive ductal carcinoma and one patient (2%) with invasive lobular carcinoma. Nine patients (17%) had stage I breast cancer, 27 (52%) had stage II cancer, 13 (25%) had stage III cancer, and three (6%) had stage IV disease.
MRI's performance
The researchers found that breast MRI visualized cancer in 52 of the 53 patients, achieving sensitivity of 98%. One cancer was missed due to marked background enhancement. The mean size of the detected lesions was 5.5 cm (± 3.0 cm; range, 1.0-13.0 cm).
As for clinical benefits, breast MRI changed the surgical management of 15 patients (28%). Among them, seven women (13%) no longer needed a lumpectomy, four (8%) required a larger lumpectomy, two (4%) had contralateral disease, and two (4%) had unsuspected metastasis.
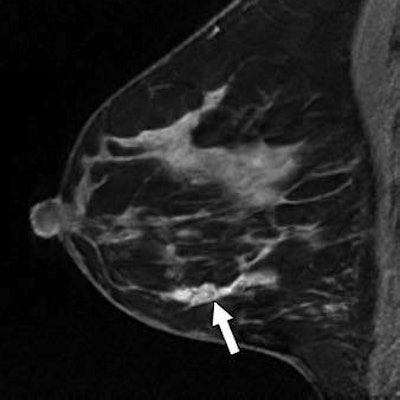
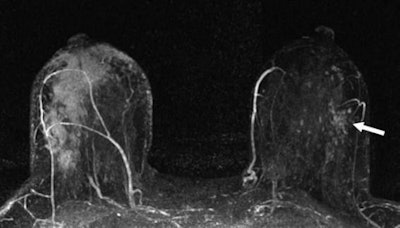 A 40-year-old woman with newly diagnosed right breast cancer presented with swelling five-months postpartum while lactating. Maximum-intensity projection MR image (above) and left breast sagittal contrast-enhanced T1-weighted MR image (below) show known multicentric inflammatory right breast cancer (arrow, above) and left breast nonmass enhancement (arrow, below) in linear distribution. MRI-guided biopsy of the left breast diagnosed ductal carcinoma in situ. Images courtesy of AJR.
A 40-year-old woman with newly diagnosed right breast cancer presented with swelling five-months postpartum while lactating. Maximum-intensity projection MR image (above) and left breast sagittal contrast-enhanced T1-weighted MR image (below) show known multicentric inflammatory right breast cancer (arrow, above) and left breast nonmass enhancement (arrow, below) in linear distribution. MRI-guided biopsy of the left breast diagnosed ductal carcinoma in situ. Images courtesy of AJR.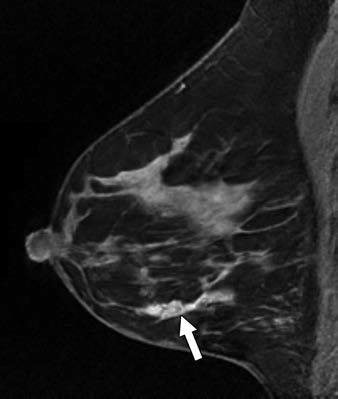
The researchers were able to compare MRI's sensitivity against that of mammography and ultrasound among 33 subjects who were imaged with all three modalities. Ultrasound led the way with sensitivity of 100% (33 of 33 lesions), followed by MRI at 97% (32 lesions) and mammography at 91% (30 lesions).
In addition, for 29 (55%) of the 53 patients, MRI showed findings indicating a larger tumor size or greater extent of cancer than seen on mammography or ultrasound. Breast MRI also indicated a tumor size at least 1 cm larger than expected based on mammography and ultrasound for 11 (21%) patients.
No deterrent to MRI
The results, Myers said, seem to oppose the notion that marked background enhancement among women undergoing breast MRI in their first postpartum year is a deterrent to diagnostic image quality.
"We still were able to see 98% of the tumors, and we were still able to detect clinically relevant additional disease in many of the patients, which impacted surgical management in 28%, even in that first year postpartum," she said.
While the results are promising for pregnancy-associated breast cancer, it may be too soon for Johns Hopkins or Memorial Sloan-Kettering to change their MR imaging strategies for these patients. Preoperative MRI scans are determined on a case-by-case basis, Myers said.
"That being said, although we don't have a strict protocol, if a patient met the description in this study, I would be very inclined to encourage the clinician that preoperative breast MRI may be very helpful, and in any case be assured that the MRI would not be limited even though the patient is in that first year postpartum," she said.