Researchers from VU University Medical Center (VUMC) in Amsterdam used functional MRI (fMRI) to visualize disruptions in several areas of the brain associated with attention and visual processing in people with Parkinson's disease. The findings could explain visual hallucinations in these patients, according to a paper published online on September 27 in Radiology.
The results indicate that while Parkinson's disease affects resting-state functional connectivity of the posterior and paracentral brain regions, visual hallucinations are associated with a more global loss of network connectivity.
"Our findings argue against the notion that a single specific functional brain region or network is the neural substrate of visual hallucinations in Parkinson's," said lead author Dr. Dagmar Hepp from VUMC's department of neurology and department of anatomy and neurosciences. "Rather, [we] supply further evidence for a more global loss of network efficiency, which could drive disturbed attentional and visual processing and thereby lead to visual hallucinations in Parkinson's."
Parkinson's hallucinations
 Dr. Dagmar Hepp from VUMC.
Dr. Dagmar Hepp from VUMC.As many as 75% of Parkinson's patients experience visual hallucinations at some point, Hepp wrote in an email to AuntMinnie.com. Naturally, the condition has a significantly negative effect on one's quality of life.
"Visual hallucinations are associated with cognitive problems and the development of dementia in Parkinson's," Hepp added. "Thus, the high prevalence and great impact of visual hallucinations in Parkinson's prompted us to investigate the underlying processes with functional MRI to gain a better understanding of the symptom and, ultimately, provide clues for therapy."
Hepp and colleagues have previously explored the nature of the cognitive problems in Parkinson's patients with visual hallucinations, comparing them with patients who did not have visual hallucinations. In those studies, the researchers found that Parkinson's patients with visual hallucinations had more severe attention and memory problems.
Previous structural MRI studies have also uncovered atrophy or shrinkage in specific brain areas of Parkinson's patients with visual hallucinations, compared with those without such hallucinations. Other papers have reported a reduction in brain volume or an increase in regional brain volume among those with Parkinson's hallucinations.
"We speculated that functional MRI, which measures the communication between brain areas, may be a more sensitive marker and may identify brain areas or networks that show dysfunction in Parkinson's patients with visual hallucinations and thereby aid in the unraveling of this frequent and troublesome symptom," Hepp said.
Cognitive function
This retrospective study included 15 Parkinson's patients with visual hallucinations, 40 Parkinson's patients with no visual hallucinations, and 15 control subjects. All participants underwent structural whole-brain 3-tesla MRI scans (Signa HDxt, V15M, GE Healthcare) with a sagittal 3D T1-weighted fast-spoiled gradient-echo sequence. The researchers were then able to calculate mean functional connectivity between 47 regions of interest and compare the results with whole-brain and region-specific activity.
Parkinson's patients were asked about the presence of visual hallucinations through the Scales for Outcomes in Parkinson Disease Psychiatric Complications (SCOPA-PC) questionnaire. A score of at least 1 on the first item classified patients as having hallucinations, while a score of 0 classified them as not having hallucinations.
In addition, cognitive capabilities were evaluated with the Mini-Mental State Examination (MMSE) and the Cambridge Cognitive Examination (CCE). The tests assess and score seven cognitive domains: orientation, language, memory, attention and calculation, praxis, abstract thinking, and perception. A CCE score of less than 80 indicates dementia, while an MMSE score of at least 24 indicates normal cognition.
Functional connectivity
In reviewing the fMRI results, the researchers discovered significant differences in whole-brain mean functional connectivity between Parkinson's patients and the control subjects (p = 0.013). Further analysis showed that only the Parkinson's patients with visual hallucinations had significantly lower whole-brain mean functional connectivity than control subjects (p = 0.010); there was no statistically significant difference between the Parkinson's patients with no visual hallucinations and control participants (p = 0.14).
In addition, Parkinson's patients with visual hallucinations had reduced functional connectivity compared with the control subjects in nine brain regions. The underperforming regions were in the frontal cortex, temporal cortex, rolandic operculum, occipital cortex, and striatum and were related to cognitive deficits.
The regional connectivity analysis showed eight regions in the occipital lobe and paracentral area where functional connectivity was less for both Parkinson's patients with and without visual hallucinations, compared with the control participants. These regions are associated with motor performance.
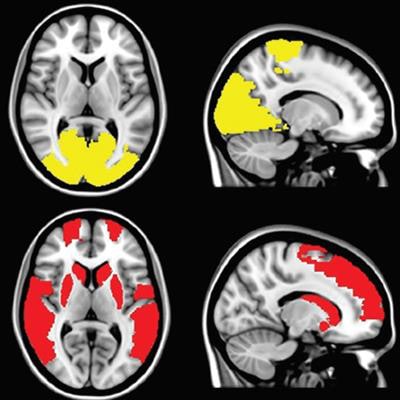
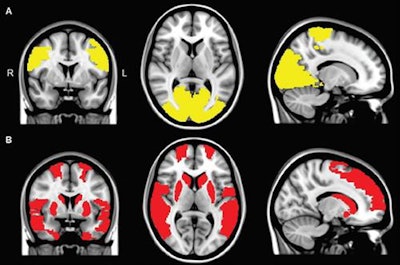 Functional MR images show reduced regional connectivity in Parkinson's patients (A) and in Parkinson's patients with visual hallucinations (B). A regional functional connectivity analysis revealed lower connectivity in patients with visual hallucinations and in patients without hallucinations, compared with control subjects, in the paracentral and occipital regions (yellow areas in A). Functional connectivity in the frontal, temporal, and subcortical regions was exclusively lower in Parkinson's patients with visual hallucinations, compared with controls (red areas in B). Images courtesy of Radiology.
Functional MR images show reduced regional connectivity in Parkinson's patients (A) and in Parkinson's patients with visual hallucinations (B). A regional functional connectivity analysis revealed lower connectivity in patients with visual hallucinations and in patients without hallucinations, compared with control subjects, in the paracentral and occipital regions (yellow areas in A). Functional connectivity in the frontal, temporal, and subcortical regions was exclusively lower in Parkinson's patients with visual hallucinations, compared with controls (red areas in B). Images courtesy of Radiology.The differences between Parkinson's patients and the controls were further detailed in the review of the cognitive tests. Global cognitive functioning scores in the CCE test were significantly lower among all Parkinson's patients than for the control participants (p = 0.004), but the results were comparable between the groups (p = 0.721) for the MMSE test.
As one might expect, Parkinson's patients with visual hallucinations performed worse on a statistically significant basis (p < 0.05) than Parkinson's patients with no visual hallucinations in orientation, language, memory, and perception on the CCE test.
Therapeutic implications
While the study provides new insights into the functional substrates of visual hallucinations in Parkinson's patients, Hepp said there are no direct therapeutic implications for patient care based on the research.
"Future studies could indicate whether techniques that could stimulate the areas with decreased connectivity in Parkinson's patients with visual hallucinations -- the areas that communicated less with the rest of the brain -- could be helpful to treat visual hallucinations in Parkinson's," she said. "In addition, our findings may offer future markers to predict the occurrence of visual hallucinations in Parkinson's patients."
Hepp and colleagues plan to continue along this research path with a longitudinal study to see whether changes in functional connectivity could indeed predict the occurrence of visual hallucinations among Parkinson's patients.
"Since the presence of visual hallucinations in Parkinson's is often associated with more severe other nonmotor symptoms, such as anxiety, depression, cognitive problems, and sleep disturbances, the presence of these symptoms should be included in such a longitudinal functional MRI analysis as well," she said.




















