Whole-body MRI is an emerging clinical tool for accurate and early assessment of oncology patients in a single, noninvasive technique, Egyptian researchers have found. It's a reliable, reproducible method that is ideal for follow-up, they added.
Based on their clinical experience, Dr. Ahmed Abdel Razek, a professor of diagnostic radiology at Mansoura Faculty of Medicine in Mansoura, and colleagues noted that whole-body MRI and whole-body diffusion-weighted MRI are great techniques for assessing oncology patients without the use of radiation or contrast administration.
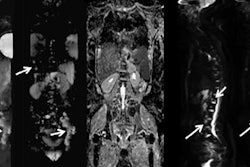
"Whole-body diffusion-weighted MR imaging provides additional functional information about tissue cellularity and intercellular water movement, and differentiation between benign and malignant tumors," they stated in an e-poster from RSNA 2017. "Malignant tumors are generally hypercellular, which show restricted water diffusion resulting in high signal intensity."
The techniques
Many oncology patients undergo different imaging examinations, such as CT, MRI, bone scans, and PET/CT. These modalities tend to be time-consuming and expensive and can have low diagnostic accuracy, while whole-body MRI does not suffer from these drawbacks, according to the authors.
Initially, whole-body MRI required short tau inversion-recovery (STIR) images of whole body regions, but that evolved into multiple sequences including T1-weighted imaging and whole-body diffusion-weighted imaging (DWI). Related, whole-body DWI with background suppression improves disease and background-tissue contrast by using high b-values, facilitating total tumor overview. Its sensitivity to bone and soft-tissue lesions makes it an alternative to bone scans and PET/CT with no radiation exposure, according to Razek and colleagues.
At their institution, they have used a 1.5-tesla MRI scanner (Ingenia, Philips Healthcare) with a combined built-in body coil and anterior coil to study whole-body MRI. Exams took between 35 and 45 minutes.
The researchers discovered whole-body DWI under breath-hold with thick slices (8 mm to 10 mm) resulted in low signal-to-noise ratio. DWI with background suppression performed with free respiration and thin slices (3 mm) had high signal-to-noise ratio.
DWI with background suppression could be used as a screening tool for the detection of any bony and soft-tissue metastasis, in evaluation of nodal involvement and staging of lymphoma, and in follow-up and treatment response monitoring. For metastasis using DWI, background tissues are relatively suppressed while most forms of tumors show restricted water diffusion, they noted.
For lymphomas, whole-body imaging allows evaluation of the full extent of disease at baseline, accurate staging, adaptation of treatment strategies, assessment of treatment response, and detection of relapse. Stage I of lymphoma involves a single lymph node region or lymphoid structure. Stage II involves more than one lymphatic region on one side of the diaphragm. Stage III involves lymph node regions on both sides of the diaphragm. Stage IV involves one or more distant extra-lymphatic organs with or without associated lymph node enlargement, continued the researchers.
Overall, they listed the following positives of whole-body DWI:
- Detects primary lesions and remote metastasis
- Valuable in therapy monitoring and follow-up
- No ionizing radiation exposure
- No contrast administration
- Evaluation of whole body by one single technique
- 3D evaluation of the whole body
- Evaluation of skeletal and soft-tissue metastasis
Limitations, however, include patient-dependent factors, foreign body artifacts, motion-related artifacts, and calcium-containing lesions.
All in all, though, Razek and colleagues concluded that whole-body MRI, including DWI background suppression, is a powerful tool in a growing number of clinical cases.