The early diagnosis of an abnormality in any part of the body is often seen as a way to speed recovery. Having an MRI scan for knee pain when symptoms begin, however, hikes healthcare costs with no great benefit to the patient's quality of life, according to a study published online April 17 in Radiology.
In a 12-month analysis, healthcare costs per patient were significantly higher for those who had MRI scans followed by standard care, compared with patients who skipped the imaging exam. While that finding alone seems obvious, the kicker is that the early MRI scan did not significantly improve quality of life or significantly reduce the number of referrals to orthopedic surgeons.
"Not to request an MR examination might be challenging in the current climate of defensive medicine, in which patients are demanding and healthcare providers have a limited amount of time," wrote the group led by Dr. Kim van Oudenaarde from Leiden University Medical Center in the Netherlands. "With the presented results, we hope to support both patients and healthcare providers in the primary evidence-based care of patients with traumatic knee symptoms."
Where does it hurt?
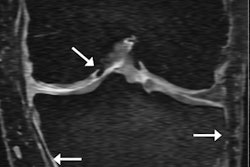
Knee pain is the second most common musculoskeletal reason for seeing a physician, and MRI is the modality of choice for diagnosing a soft-tissue lesion. Previous studies have shown that MRI can achieve sensitivity of 87% and specificity of 93% for the overall detection of meniscus and anterior cruciate ligament tears. In addition, the modality's high rate of diagnostic accuracy has made arthroscopy obsolete in many cases, the authors noted (Radiology, April 17, 2018).
"However, due to the lack of evidence regarding the added value of MRI in primary care, the Dutch College of General Practitioners guidelines recommend not to request MRI in these patients," van Oudenaarde and colleagues wrote. "Other countries have developed similar guidelines that provide conflicting or unclear advice regarding when to perform MR imaging in primary care or when to refer a patient to an orthopedic surgeon."
To test the value of referring people with knee pain for an early MRI scan, the researchers recruited patients 18 to 45 years old between October 2012 and December 2015 who went to their physician for knee pain due to an injury, loss of function, or both. Patients were excluded if they were already receiving care for their symptoms, had previously undergone surgery on the affected knee, or had fractures, osteoarthritis, or contraindications to MRI, among other criteria.
"The age criterion [of younger than 45 years] was chosen to exclude subjects with a relatively higher prevalence of degenerative findings for which no clear treatment options are currently available," the authors explained.
To MRI or not to MRI?
The final cohort of 356 patients had a mean age of 33 (± 8) years. The researchers divided the subjects into two groups: standard care or MRI with standard care.
The standard care group was treated according to guidelines that included rest or specific exercises, pain medication, and physiotherapy. Physicians were asked to refer their patients to an orthopedic surgeon if treatment was unsuccessful but not to request an MRI.
Subjects in the MRI group had scans within two weeks of completing the first in a series of questionnaires, in addition to receiving standard care. The subjects underwent a 1.5-tesla MRI scan with a dedicated knee coil at one of six different imaging centers.
To assess quality-adjusted life years (QALYs), the researchers asked the subjects to fill out surveys at the start of the study, at six weeks, and at three, six, nine, and 12 months based on the previous three months of healthcare expenses. Healthcare costs included visits to a physician and/or orthopedic surgeon, therapy sessions, MRI scans, other imaging exams, arthroscopy, any hospital admission, and medication.
The participants also recorded costs that weren't related to medical care, including lost time and wages from being away from work, housekeeping, family caregiving, traveling, and additional items such as knee braces or crutches.
At the 12-month follow-up, the researchers found significantly higher healthcare costs per patient in the MRI group than in the standard care group. Nonhealthcare costs were only slightly higher in the MRI group.
| Costs of early MRI and standard care for knee pain | |||
| MRI and standard care | Standard care only | Mean difference | |
| Healthcare costs | 1,109 euros ($1,375) | 837 euros ($1,038) | 273 euros ($338) |
| Nonhealthcare costs | 4,526 euros ($5,612) | 4,224 euros ($5,237) | 302 euros ($374) |
| Total | 5,635 euros ($6,987) | 5,061 euros ($6,275) | 575 euros ($713) |
"This difference [in healthcare costs] was mainly based on higher costs of MR imaging and on insignificantly higher costs of physiotherapy and arthroscopy in the MR group," the authors wrote. "[The] higher nonhealthcare costs were mainly based on higher costs for work absenteeism in the MRI group, with a mean of 10.3 absent workdays in the MRI group compared with 7.8 absent workdays in the usual care group (p = 0.188)."
Despite the greater cost of undergoing an early MRI scan, there were no significant differences in mean quality-adjusted life years over the 12-month follow-up period. Patients who had an MRI scan had a mean QALY of 0.888, compared with a mean QALY of 0.899 for the usual care group.
In other findings, more patients in the MRI group underwent arthroscopy (22%, compared with 16% in the standard care group), but the difference was not statistically significant (p = 0.150).
"From the cost-utility analyses, we concluded that referral for early MR imaging by the general practitioner is unlikely to be cost-effective compared with usual care in patients aged 18 to 45 years with traumatic knee symptoms," van Oudenaarde and colleagues wrote.
The findings can be applied to other healthcare systems, the authors noted, where "healthcare providers other than orthopedic surgeons are involved in the primary care and diagnostic workup of patients with symptoms after a traumatic knee injury."