Could the treatment of brain tumors with radiation therapy contribute to the amount of gadolinium deposition in the brains of children who have received gadolinium-based contrast agents (GBCAs) during MRI scans? That's the implication of a new study published in the May issue of Radiology.
Researchers from Children's Hospital Los Angeles postulated that structural changes caused by brain tumors -- as well as treatment of the tumors with radiation -- could be a major contributing factor to how much gadolinium ends up deposited in the brains of children who receive GBCAs -- regardless of how much contrast is administered.
 Dr. Benita Tamrazi from Children's Hospital Los Angeles.
Dr. Benita Tamrazi from Children's Hospital Los Angeles.The findings could shift the debate over the cause of gadolinium deposition, which has begun to focus on disruption to the blood-brain barrier as a possible cause of the phenomenon.
"The findings shift our direction when it comes to gadolinium deposition," said lead author Dr. Benita Tamrazi, an assistant professor of pediatric neuroradiology at Children's Hospital. "We initially thought that the gadolinium we give all went to the brain. Now it is clear that other factors are at play, and there may not be dose dependence. Now we need to ask some more questions."
Linear vs. macrocyclic
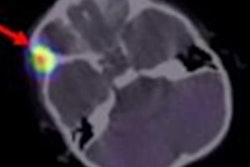
The current controversy over gadolinium deposition began in December 2013, when Kanda et al published findings that indicated that patients who received GBCA contrast had elevated signal intensities in the brain's dentate nucleus and globus pallidus regions on unenhanced T1-weighted MRI scans. Clinicians began to switch to macrocyclic GBCAs when follow-up research indicated that this class of agents resulted in less deposition than linear GBCAs.
Even with those findings in hand, Tamrazi, as a neuroradologist, saw inconsistent results in her pediatric cancer patients undergoing irradiation or chemotherapy who underwent given GBCA-enhanced MRI scans.
"I read these MRIs every day, and I was noticing that I didn't see [signal intensity] changes consistently in these patients," she told AuntMinnie.com. "Even in pediatric patients whose doses [of GBCA] were higher -- like 15 to 20 doses of the contrast media -- I was not seeing the changes, but in five to 10 doses of the contrast agent I was seeing the [signal intensity] changes."
Right away, she sensed something may be amiss because signal intensity increases did not always parallel GBCA exposure. An additional concern is the young patient population itself. Pediatric cancer patients are likely to undergo multiple GBCA-enhanced MRI scans over the course of their disease.
"We also noticed that previous papers did not do a subanalysis of pediatric patients who received radiation, compared to pediatric patients who receive no radiation for the differences in signal intensity that we are seeing," she said. "I had to look at the unconfounded data to see if there is a difference in signal intensity based on gadolinium with radiation and gadolinium without radiation. The answer is yes."
Pediatric strategies
For this study, Tamrazi and colleagues reviewed GBCA-enhanced MRI scans among their pediatric cancer patients undergoing treatment between 2000 and the first half of 2015 (they excluded MRI scans during and after July 2015, when the hospital switched to a macrocyclic GBCA). The 144 subjects included children younger than 18 years of age and who had undergone at least four contrast-enhanced MRI brain scans with the linear GBCA gadopentetate dimeglumine (Magnevist, Bayer HealthCare) (Radiology, May 2018, Vol. 287:2, pp. 452-460).
MRI exams for all subjects were performed on either a 1.5- or 3-tesla system (Achieva, Philips Healthcare) and included an unenhanced axial T1-weighted sequence in the form of a fluid-attenuated inversion-recovery (FLAIR) or an unenhanced T1-weighted 3D sequence.
The researchers then divided the subjects into four groups:
- 55 patients (mean age 9.8 years at first MRI scan; mean of 16.8 GBCA exposures) received radiation therapy for their tumors
- 19 patients (mean age 5.5 years at first MRI scan; mean 20.3 GBCA exposures) whose tumors were treated only with chemotherapy
- 52 patients (mean age 7.9 years at first MRI, mean 10.0 GBCA exposures) whose tumors were not treated
- 18 patients (4.4 years at first MRI scan; mean 8.7 GBCA exposures) had a neuroblastoma but no central nervous system (CNS) disease
The team performed signal intensity calculations for regions of interest (ROIs) within the globus pallidus, thalamus, dentate nucleus, and pons (mean of 5 mm; range, 4-8 mm) on unenhanced axial T1-weighted MR images for all patients. The researchers then compared signal intensities based on the patients' ages, number of GBCA doses, along with the dentate nucleus-to-pons and globus pallidus-to-thalamus ratios from the children's most recent MRI scans.
Relevant ratios
The dentate nucleus-to-pons ratio differed significantly among the four study groups (p = 0.007). Individually, the ratio in the radiation therapy group was significantly greater than the nontreated group and the neuroblastoma group (p < 0.05) but not greater than that in the chemotherapy-only group. The researchers also found no statistically significant difference in the ratios among the chemotherapy-only group, the nontreated group, and the neuroblastoma group.
The globus pallidus-to-thalamus ratios differed significantly among the groups (p < 0.0001), with the ratios in the radiation therapy group, chemotherapy-only group, and the nontreated brain tumor group significantly greater than that in the neuroblastoma group.
| GBCA signal intensity ratios by type of patient group | ||||
| Ratio | Nontreated | Chemotherapy only | Neuroblastoma | Radiation therapy |
| Dentate nucleus-to-pons ratio | 1.03 ± 0.02 | 1.06 ± 0.02 | 1.04 ± 0.02 | 1.1 ± 0.02 |
| Globus pallidus-to-thalamus ratio | 1.17 ± 0.01 | 1.17 ± 0.01 | 1.08 ± 0.01 | 1.19 ± 0.01 |
When the researchers compared signal intensities to GBCA doses, they discovered the only statically significant difference was in the dentate nucleus-to-pons ratio among patients who did not receive any radiation or chemotherapy. As the number of GBCA exposures increased from fewer than 10 to more than 20, their signal intensity elevated (p < 0.001).
By comparison, the team found no statistically significant difference in signal intensity among the patients in the globus pallidus-to-thalamus ratio regardless of the number of GBCA doses.
In their comparison of all four groups, the researchers found the dentate nucleus-to-pons ratio to be significantly higher in the radiation therapy group than the nontreated group when both sets of patients received fewer than 10 GBCA administrations (p < 0.001). Interesting, the results were reversed when the same two groups received more than 20 GBCA doses; the nontreated group had a significantly greater dentate nucleus-to-pons ratio than the radiation therapy group (p < 0.05).
Questions remain
"Our study demonstrated that the presence of primary brain disease, specifically primary brain tumors, plays a significant role in T1 hyperintensity, more so than the administration of linear GBCAs alone, because the patients with brain tumors in our study had [signal intensity] changes that were different from patients who received gadolinium but who did not have a primary brain tumor," the authors wrote.
As seems to be the case over the last few years, research into gadolinium retention and deposition can raise more questions than it solves.
"Do we know everything about gadolinium deposition? Absolutely not," Tamrazi said. "We really don't know much about what is depositing, what is the mechanism is, or what it means for the long term. Our studies basically show a lot of the initial data that signal intensity might not be dose-dependent. There might be other factors, and we need to start looking at that in these specific patients."
Tamrazi and her colleagues are continuing their study into gadolinium deposition and potential signal intensity changes with macrocyclic GBCA gadobutrol (Gadavist, Bayer) on the brains of pediatric cancer patients undergoing irradiation or chemotherapy. The study was recently accepted for publication. In the meantime, she advises her fellow neuroradiologists and clinicians to remain vigilant.
"My advice would be to remain cautious and keep in mind that there is still so much uncertainty regarding gadolinium deposition in the brain," Tamrazi added. "I think [clinicians] need to be aware of the fact that most of these changes have been described in brain tumor patients receiving multiple doses and that there may be other variables at play that influence the signal changes."
Study disclosures
Bayer HealthCareprovided financial support for the researchers to study the effect of intravenous gadolinium chelate administration in the pediatric population at Children's Hospital Los Angeles. The authors had control of the data and the information submitted for publication, according to Tamrazi et al.


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)