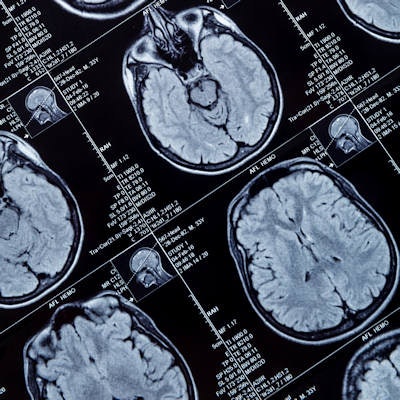
By performing an MRI scan soon after traumatic brain injury (TBI), clinicians can more quickly gather prognostic information based on the type and specific location of the injury, according to a study by researchers from Saudi Arabia and published in the Journal of Affected Disorders.
The most common result of severe head trauma is a diffuse axonal injury, which is associated with varying degrees of post-traumatic amnesia, loss of consciousness, hospital stays, and poor neurocognitive outcome. While those outcomes are often unavoidable, early detection of the injury's location is paramount to determining treatment and the patient's prognosis.
"MRI in the early subacute stage can accurately detect the presence of diffuse axonal injury and precisely localize its location," wrote the researchers, led by Dr. Nasser Aldossary from Prince Sattam Bin Abdulaziz University in Alkharj (J Affect Disord, September 5, 2018). "Early detection of them will help professionals to start strategic therapeutic plans to avoid or at least ameliorate the effects of these potentially serious complications."
While MRI has proved more sensitive for detecting diffuse axonal injury lesions, few studies on patients with TBI have focused on the radiological and clinical factors associated with the neurocognitive and psychiatric outcomes, according to the study authors.
The researchers analyzed 251 patients between the ages of 18 and 60 who were admitted with severe head trauma to one of three Saudi Arabian hospitals from 2014 through 2017. Patients underwent conventional 1.5-tesla MRI scans (Optima MR450w, GE Healthcare) within the first month after the injury and also an assessment of cognitive function using the Mini-Mental State Examination (MMSE). MR images revealed 181 patients (72%) who had evidence of diffuse axonal injury, compared with 70 patients (28%) with no evidence of this type of injury.
Patients with a diffuse axonal injury had significantly longer durations of post-traumatic amnesia and hospital stays, as well as more significantly adverse cognitive issues. However, the researchers found no significant difference in duration of the period of loss of consciousness between the two patient groups.
| Impact of diffuse axonal injury on outcomes of patients with TBI | |||
| Patients with no diffuse axonal injury | Patients with diffuse axonal injury | p-value | |
| No. of subjects | 70 | 181 | |
| Mean duration of loss of consciousness | 44.03 hours | 47.71 hours | NS |
| Mean duration of post-traumatic amnesia in weeks | 2.69 weeks | 6.23 weeks | < 0.001* |
| Mean length of hospital stay | 15.65 days | 16.50 days | 0.034* |
| Mean MMSE score | 21.81 | 10.62 | < 0.001* |
* Statistically significant
"The vast majority of recovery after TBI occur in the two years after brain injury," Aldossary and colleagues noted. "After this, the brain injured patient faces an uncertain future."
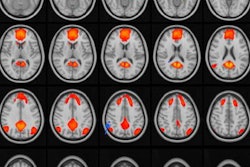
The location of the diffuse axonal injuries also played a major role in a patient's recovery time, with the cerebral hemisphere and associated areas contributing greatly to the severity of the condition and length of recovery.
"In subgroup analysis, we noticed that patients with cerebral hemisphere and brainstem lesion and patients with mixed lesions had the worst cognitive impairment, while patients with isolated cerebral hemisphere lesion had the best outcome," they concluded.



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











